Abstract
Background: Successful medical-dental integration is key to achieving children’s health equity. In 2015, a community health center (CHC) in Boston, Massachusetts, implemented a model of interdisciplinary care in a nationwide pilot. Based on the Oral Health Delivery Framework, pediatricians were trained to assess dental caries risk and apply fluoride varnish. They were trained to offer education materials to patients, incorporate oral health assessment in pediatric practice, and document preventive dental care in the electronic health record. This study assessed the level of medical-dental integration achieved by the pilot and maintained over 2 years after program implementation.
Methods: Deidentified data were provided by the CHC on all well-child visits during 2014 to 2018 for children 72 months or younger, including appointment dates, age, ethnicity, race, insurance status, and outcomes of interest (ie, whether a dental assessment was performed and whether fluoride varnish was applied). Outcomes were stratified by visit year to allow pilot (2015-2016) outcomes to be compared to pre-pilot (2014) and post-pilot (2017-2018) outcomes. Descriptive statistics were used to summarize the data.
Results: Pediatricians performed fluoride varnish applications and dental assessments in 25% and 0% of visits, respectively, at baseline; in 50.2% and 49.4% of visits, respectively, at the pilot’s end; and in 56.7% and 57.3% of visits, respectively, 2 years post-pilot.
Conclusions: The proportion of well-child visits during which pediatricians integrated oral health preventive measures increased by roughly 25% to 50% from baseline (2014) to the end of the pilot (2016) and by at least 5% from 2016 to 2018. The success of this medical-dental integration pilot underscores the need for broader implementation of interprofessional education and practice to promote children’s health equity.
Oral Health Care Is Health Care
Dental caries is the most common chronic disease of childhood, although it is largely preventable. Caries incurs short- and long-term negative health effects and can diminish both children’s and parents’ quality of life.1 Moreover, dental caries inequitably affects racially and ethnically minoritized children and children from families with low income.2 Medical and dental clinicians have an ethical obligation to respond to the inequitable distribution of dental disease as a matter of social justice.3
Oral health is key to children’s overall health. Since young children visit pediatricians or family medicine physicians more often than dentists, those physicians need to be allies in promoting oral and overall health equity.4 The American Academy of Pediatrics (AAP) issued a revised policy statement in 2014 that emphasizes medical-dental integration: “Because dental caries is such a common and consequential disease process in the pediatric population, it is essential that pediatricians include oral health in their daily practice of pediatrics.”5 The AAP also recommends that pediatricians provide anticipatory guidance about caries, perform dental assessments, instruct patients and their parents about at-home oral hygiene practice, and apply fluoride varnish during routine well-child visits.6 In 2011, the Institute of Medicine’s report, Advancing Oral Health in America, recommended changing payment policies and expanding physicians’ oral health competencies.7
Integrating pediatric health services. The Health Resources and Services Administration (HRSA) calls for multidisciplinary team practice in US health care and for infrastructure innovation to implement and evaluate oral health competencies in primary care practice.8 Medicaid programs in all 50 states and the District of Columbia reimburse physicians for fluoride applications,9 as do most private insurers, but few Medicaid programs and insurers cover oral health patient education or counseling.10 An added challenge for the creation of successful multidisciplinary teams is that medical education provides very little training focused on oral health.11 In the past 10 years, however, interprofessional standards have been included for the accreditation of educational programs in physical therapy, allied health, nursing, pharmacy, and—most recently—medicine and dentistry.11,12
Models. Medical-dental education partnerships exist, and some oral health content has been incorporated in medical education,13 but collaborative interdisciplinary team interactions need to become common. Hummel et al, with funding from Qualis Health, convened an expert panel to develop the Oral Health Delivery Framework (see Figure).14 The framework prompts clinicians to identify oral health risk factors by asking patients questions about their oral hygiene, diet, health conditions, and symptoms and to visually screen for oral health problems. Clinicians then decide whether the findings are normal and, if not, they intervene as indicated (eg, provide a referral, apply fluoride varnish). Finally, clinicians should document findings as structured data that can be utilized for decision support and for improving care management. This framework is endorsed by several organizations, including the American Academy of Nursing, the American Academy of Pediatrics, and 17 others.14,15
Figure. Oral Health Delivery Frameworka
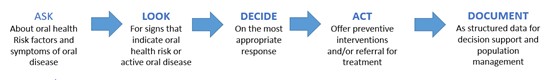
a Adapted from Hummel et al.14 Adapted with permission of Jeffrey Hummel.
The framework was piloted in 5 states at 19 US sites serving diverse patients, including community health centers (CHCs) and private clinics, by 80 teams of clinicians who received training and support.15 The program incorporated oral health assessments and fluoride application for patients 0 to 72 months of age in the workflow of the pediatric department using an approach similar to how clinicians screen patients for asthma, diabetes, cardiovascular disease, obesity, and mental illness. Pilot outcomes included 13 771 oral health assessments, 4518 fluoride applications, and 1255 referrals to patients who did not have a dental care home. As reported by Hummel et al, during the pilot, one CHC in Boston, Massachusetts, showed an 80% increase in the number of patients receiving oral health assessments during the first 14 months, a proportion that declined to 60% between months 14 and 17.15
The purpose of this article is to examine the outcomes of this CHC’s interdisciplinary program by comparing the proportion of well-child visits in which oral health services were provided during the years 2015-2016 (when the pilot was conducted at this site) to the proportion of such visits during the year 2014 (before the pilot was implemented) and during the years 2017 to 2018 (after the pilot concluded).
Methods
Participants. The sample consisted of 1456 patients who were 72 months of age or younger and who had at least one well-child visit during 2014 to 2018. The population served at the site in this study is presumed to be representative of the population that generally seeks health at community health centers.
Data collection. The data used in this study were obtained from patient records of 6949 well-child visits from 2014 to 2018 at an urban CHC and were deidentified prior to being provided to the research team. The variables extracted from the data include outcomes (ie, whether a dental assessment was conducted and fluoride varnish applied), dates of service, and the child’s date of birth, ethnicity, race, and insurance status. A total of 633 records were excluded from the analysis because they were missing the child’s date of birth.
Statistical analysis. Outcomes were stratified by visit year to allow pilot (2015-2016) outcomes to be compared to pre-pilot (2014) and post-pilot (2017-2018) outcomes. Descriptive statistics (frequencies, percentages) were used to summarize the data. All analyses were conducted using SAS statistical software version 7.1.
Results
Table 1 shows a total of 6949 visits, with appointments distributed evenly between 2014 and 2018. In most appointments, patients were younger than 12 months old, perhaps because well-child visits are recommended more frequently in the early months of life.
| Characteristic | No. (%) of Visits |
|---|---|
| Appointment year | |
| 2014 | 1359 (19.6%) |
| 2015 | 1327 (19.1%) |
| 2016 | 1446 (20.8%) |
| 2017 | 1407 (20.2%) |
| 2018 | 1410 (20.3%) |
| Age (months) | |
| 0-11 | 2983 (47.2) |
| 12-23 | 1691 (27.6) |
| 24-35 | 591 (9.4) |
| 36-47 | 552 (8.7) |
| 48-71 | 499 (7.9) |
| Race | |
| Unreported/Refused to report | 4104 (60.5) |
| African American | 2473 (35.6) |
| White | 197 (2.8) |
| Other (PI/AI/AN/other race) | 71 (1.0) |
| Ethnicity | |
| Hispanic | 2605 (37.5) |
| Non-Hispanic | 2217 (32.0) |
| Unknown | 2127 (30.6) |
| Sex | |
| Male | 3485 (50.0) |
| Female | 3464 (49.9) |
| Insurance | |
| Massachusetts Health | 5151 (74.1) |
| Private | 1687 (24.3) |
| No insurance | 111 (1.6) |
|
Abbreviations: PI, Pacific Islander; AI, American Indian; AN, Alaska Native.
|
|
Between 2014 and 2018, pediatric teams performed 2581 dental assessments and 3301 fluoride varnish applications. Table 2 shows a substantial increase in the number of well-child visits during which oral health services were provided between 2014 (the pre-pilot period) and 2015 to 2016 (the pilot period). The proportion of visits during which pediatricians performed oral health assessments increased from 0% in 2014 to 18.8% in 2015 and to 49.4% in 2016. Moreover, the proportion of visits during which pediatricians performed assessments increased to 57.5% between 2016—the last year of the pilot—and 2017 and remained relatively constant at 57.3% between 2017 and 2018. Findings from the analysis show similar gains in the proportion of appointments during which fluoride varnish was applied. While fluoride varnish was applied in 25% of well-child visits prior to the pilot (2014), it was applied in 49.7% and 50.2% of appointments during 2015 and 2016, respectively. Post-pilot, fluoride varnish was applied in 55.2% of appointments during 2017 and in 56.7% of appointments during 2018.
| Group | Well-Child Visits | ||||
|---|---|---|---|---|---|
|
All children |
2014 |
2015 |
2016 |
2017 |
2018 |
|
Fluoride application, % |
25.0 |
49.7 |
50.2 |
55.2 |
56.7 |
|
Oral health assessment, % |
00.0 |
18.8 |
49.4 |
57.5 |
57.3 |
|
Children > 11 mo. |
2014 |
2015 |
2016 |
2017 |
2018 |
|
Fluoride application, % |
46.3 |
86.4 |
94.6 |
94.1 |
96.0 |
|
Oral health assessment, % |
00.0 |
31.7 |
87.8 |
95.8 |
95.8 |
Oral health assessments and fluoride applications are recommended after 12 months of age or after first tooth eruption. When children younger than 11 months are excluded from the analysis, the proportion of appointments during which pediatricians applied fluoride increased from 46.3% (pre-pilot) to 96.0% (2 years after the pilot). The number of appointments during which pediatricians conducted oral health assessments for children older than 11 months also increased. Although no oral health assessments were reported before the pilot, oral health assessments occurred in 31.7% of appointments in 2015, in 87.8% of appointments in 2016, and in 95.8% of appointments occurring within 2 years of the pilot’s completion.
Persistent Barriers
Since implementing the pilot, the CHC has integrated its medical and dental records, enabling consultation between medical and dental teams; hired a pediatric dentist; and required oral health training for current and new clinicians.16 Yet barriers to medical-dental integration persist, including lack of insurance reimbursement for oral health services not provided by dentists, lack of oral health training for physicians, and lack of record sharing.17,18 Patients who seek care at CHCs often have minoritized racial and ethnic identities, have low incomes, and experience inequitably high risk for oral and general health problems that must be addressed during time-limited clinical encounters.17,18 Despite these barriers, this pilot points a way forward for medical-dental integration to better respond to pediatric health inequity.
Conclusions
Oral health has been defined as an integral component of general health,19 and the impact of oral health conditions on systemic health has been widely documented. Oral health problems lead to avoidable deficits in nutrition, speech development, and self-esteem, as well as to elevated dental treatment costs.18,19,20,21,22 As mentioned earlier, the incidence of dental caries is significantly higher among those from underrepresented ethnic backgrounds and those living in poverty compared to their White counterparts or those living above the federal poverty level.2 Since patients from these populations often seek care at CHCs and other safety net institutions, they are an ideal venue to implement the Oral Health Delivery Framework.22,23 This study demonstrated that in the presence of institutional commitment and with necessary support, such as that offered by HRSA and Qualis, successful programs for medical-dental integration can be implemented and maintained over time, ultimately contributing to the reduction of oral health disparities among underserved populations.
Incorporating a medical-dental integration program in routine pediatric care requires an initial investment of time and training. In Massachusetts, preventive oral health training is provided free of charge by the Department of Public Health. The Smiles for Life24 online training platform is also free of charge. It takes approximately 2 minutes of pediatricians’ time to do an oral health assessment and apply fluoride varnish and costs $1.00 for supplies.25 Even if preventive oral health care for children were more costly or time consuming, ethics and equity demand changes in practice and policy, as well as follow-up research on integrated medical-dental care for children.
References
- Park JS, Anthonappa RP, Yasar R, King NM, Martens LC. Oral health-related quality of life changes in children following dental treatment under general anaesthesia: a meta-analysis. Clin Oral Investig. 2018;22(8):2809-2818.
- Henshaw MM, Garcia RI, Weintraub JA. Oral health disparities across the life span. Dent Clin North Am. 2018;62(2):177-193.
- Ramos-Gomez F. Understanding oral health disparities in the context of social justice, health equity, and children’s human rights. J Am Dent Assoc. 2019;150(11):898-900.
-
Committee on Practice and Ambulatory Medicine; Bright Futures Periodicity Schedule Workgroup. 2017 recommendations for preventive pediatric health care. Pediatrics. 2017;139(4):e20170254.
-
Segura A, Boulter S, Clark M, et al; American Academy of Pediatrics Section on Oral Health. Maintaining and improving the oral health of young children. Pediatrics. 2014;134(6):1224-1229.
- Croke LM. Preventive pediatric health care: updated recommendations from the AAP. Am Fam Physician. 2017;96(12):814-815.
-
Institute of Medicine. Advancing Oral Health in America. National Academies Press; 2011.
-
Networks for oral health integration within the maternal child health safety net. Health Resources and Services Administration. Accessed November 16, 2021. https://www.hrsa.gov/grants/find-funding/hrsa-19-053
-
Reimbursing physicians for fluoride varnish. Pew Charitable Trusts. August 29, 2011. Updated April 6, 2017. Accessed October 5, 2021. https://www.pewtrusts.org/en/research-and-analysis/articles/2011/08/29/reimbursing-physicians-for-fluoride-varnish
-
Oral Health Initiative. Oral health reimbursement chart. American Academy of Pediatrics; 2018. Accessed November 16, 2021. https://downloads.aap.org/AAP/Excel/OralHealthReimbursementChart.xlsx
- Ferrule A, Silk H, Savageau JA. Teaching oral health in US medical schools: results of a national survey. Acad Med. 2011;86(2):226-230.
- Hamil LM. Looking back to move ahead: interprofessional education in dental education. J Dent Educ. 2017;81(8):eS74-eS80.
- Donoff RB, Daley GQ. Oral health care in the 21st century: it is time for integration of dental and medical education. J Dent Educ. 2020;84(9):999-1002.
-
Hummel J, Phillips KE, Holt B, Hayes C. Oral health: an essential component of primary care. Qualis Health; June 2015. Accessed July 26, 2021. https://oralhealth.hsdm.harvard.edu/files/oralhealth/files/white-paper-oral-health-primary-care.pdf?m=1498575004
-
Hummel J, Phillips KA, Holt B, Virden M; Safety Net Medical Home Initiative. Organized, evidence-based care: oral health integration. Qualis Health; October 2016. Accessed October 5, 2021. https://www.safetynetmedicalhome.org/sites/default/files/Guide-Oral-Health-Integration.pdf
-
Zea A. The Role of Electronic Records in the Integration of Oral Health and Primary Care Services in Community Health Centers. Dissertation. Boston University; 2020.
-
Harnagea H, Couturier Y, Shrivastava R, et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ Open. 2017;7(9):e016078.
-
Bernstein J, Gebel C, Vargas C, et al. Integration of oral health into the well-child visit at federally qualified health centers: study of 6 clinics, August 2014-March 2015. Prev Chronic Dis. 2016;13:E58.
- Ismail AI, Hashim Nainar SM, Sohn W. Children’s first dental visit: attitudes and practices of US pediatricians and family physicians. Pediatr Dent. 2003;25(5):425-430.
- Wysen KH, Hennessy PM, Lieberman MI, Garland TE, Johnson SM. Kids get care: integrating preventive dental and medical care using a public health case management model. J Dent Educ. 2004;68(5):522-530.
- Jones JA, Snyder JJ, Gesko DS, Helgeson MJ. Integrated medical-dental delivery systems: models in a changing environment and their implications for dental education. J Dent Educ. 2017;81(9):eS21-eS29.
- Jones E, Shi L, Hayashi AS, Sharma R, Daly C, Ngo-Metzger Q. Access to oral health care: the role of federally qualified health centers in addressing disparities and expanding access. Am J Public Health. 2013;103(3):488-493.
-
Paradise J, Rosenbaum S, Markus A, et al. Community health centers: recent growth and the role of the ACA. Kaiser Family Foundation. January 18, 2017. Accessed March 9, 2018. https://www.kff.org/report-section/community-health-centers-recent-growth-and-the-role-of-the-aca-issue-brief/
-
Smiles for Life. Accessed November 16, 2021. https://www.smilesforlifeoralhealth.org/
- Silk H, Deutchman M. Offering oral health services in your office. Fam Pract Manag. 2014;21(4):21-24.