Abstract
In this moment of pandemic and social unrest, health workers feel overwhelming exhaustion, uncertainty, and powerlessness. At the same time, a deep spirit of resilience and a desire for innovation, discovery, and justice compel health workers to retain their commitment to serving patients and communities. This essay takes this context into consideration and proposes pragmatic steps toward a reimagined and reinvigorated future for our work as health workers.
Learning the Art of Patient Distance
Long before a barbed virus would so thoroughly upend our lives, I bought my first stethoscope in 2001. With this symbol of tremendous power around my neck, I sought a career of proximity to patients’ lives. Proximity, however, wasn’t something I would learn. My first lessons in medical school were with cadavers and pathology slides. When I started conversing with patients, my teachers handed me a formulaic script that largely avoided their personal lives and social context. In residency, I learned to provide more patient care in less time and that sharing who I was with patients was risky and unprofessional. I absorbed that medical care happens on our terms in our spaces; outside of 3 home visits, all my patient encounters were inside hospitals and clinics.
Learning the Art of Personal Distance
I learned to auscultate by listening to the hearts of classmates, patient-actors, and, eventually, patients. Curiously, never did I learn to listen to my own heart, in more ways than one. I never examined how my story as a White man who grew up in rural Minnesota as the descendant of German, Irish, and French settlers might affect patient care. I never considered how the illness narratives of my upbringing or the culture of biomedicine shaped my assumptions about health. With my stethoscope’s bell continuously pointed away from myself on a longer and longer tether, I became skilled at maintaining distance from the social context of both myself and my patients.
Inventing Distance
René Laënnec, a White European, invented the stethoscope in 1816 not because it generated clearer heart sounds but because it eased the discomfort of gendered social norms. Clinicians at that time sought freedom from the muddying interference of social context, economic pressures, and political ideology to purify objective recognition of disease.1 Stethoscopes supported these efforts by amplifying bodily sounds over the distracting background of patient voice.
Today, as a primary care physician, I continue clinging tightly to my stethoscope while participating in systems that perpetuate distance. Hurried encounters force us clinicians to interrupt patients. Electronic medical records dominate our attention and distract from human interaction. Telehealth eliminates physical presence, which risks creating isolation and disconnectedness. Billing tallies the use of the stethoscope and other distancing tools, not whether a clinician listened well to human stories.
Consequences of Distance
Our continuous pursuit of distance costs us clinicians a great deal. Meaningful opportunities for human connection are lost. During a recent clinic visit with me, a patient who moved to Minnesota from Vietnam in the 1980s started weeping about her husband’s death from pulmonary fibrosis. She quickly stopped, however, wiped her tears, and said, “I’m sorry I’m wasting your time.” Thirty years in our health system had taught her that clinicians considered her emotional and relational life to be a waste of their time.
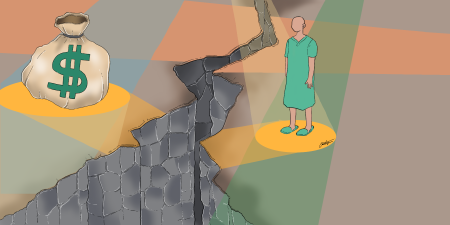
With distance, we blame patients for their conditions instead of seeing the oppressive social forces that sicken humans. I recently spent an entire clinic visit preaching antiviral medication adherence to a 50-year-old male born in Myanmar with a rising hepatitis B viral load. Only later did I learn that high-deductible insurance paired with a low-paying job made purchase of the medication impossible for him.
With distance, we blame patients for their conditions instead of seeing the oppressive social forces that sicken humans.
We avoid examining our complicity in reproducing harmful social forces. We miss how we uphold White supremacy through race-based adjustments of estimated glomerular filtration rate and spirometers.2 We ignore our control and marginalization of people experiencing homelessness, imprisonment, and forced migration.3 Honestly mirroring the ableism of our systems, a middle-aged female born in Myanmar recently asked me in clinic, “Am I normal?” Puzzled, I asked for clarification, and she responded, “Every time I come in you tell me something is wrong with me.”
Indeed, the clinic walls and our hearts are not impermeable to social context. Since the stethoscope’s invention, racism, racial capitalism, patriarchy, and ableism have both originated within and penetrated the clinic. Instead of confronting this history head-on, we continuously lengthen the tubing of our stethoscopes, thereby disconnecting ourselves from patients and undermining our desire to reduce suffering and heal.
Pursuing Proximity
How and where might we look in order to reverse course? To start, we could make the radical about-face of turning our stethoscopes upon ourselves. Somatic therapists urge connection first with our own bodies in order to begin healing disconnection and dehumanization.4 Integrating embodied practices, such as palpating our own pulsating hearts or tightened abdominal walls as we provide clinical care, generates stamina for honestly grappling with the privileges, biases, trauma, and strengths in our own stories.
With settled bodies, we are then ready for transformational connection with patients and communities. We practice narrative health. We ask about and affirm patients’ resilience and strength. We learn history from the perspective of Black, Indigenous, and other historically oppressed communities. With those voices in mind, we walk around our own neighborhoods and those of our patients. We do home visits. We coordinate care with community organizations working on affordable housing, food security, and immigration. We learn from and refer to other healing traditions. We seek out community artists who reveal insights that no randomized control trials ever can. We accompany community health workers. We learn from nurses who organize collectives. We engage with and keep engaging with racial justice training. We take a social medicine course and then teach one. We communicate with and testify in front of elected officials. We work to integrate health care into emerging solidarity economies.
Incorporating these ideas into health work is not new. In the United States, somatic therapists are actively creating a global network to heal embodied trauma.5 In Cuba, medical students visit thousands of homes to prepare for careers living and working in the same neighborhoods as their patients.6 In Rwanda, physicians support a national network of community health workers who provide frontline care.7 Clearly, we are not short on the imagination needed for pragmatic and visionary solutions. What we have lacked is the courage and the will to collectively turn around on the well-worn path of distance that medicine has traveled.
A Portal
Amidst the disruptive twinning of the COVID-19 pandemic and protests demanding racial justice, we stand facing what has aptly been described by Arundhati Roy as a portal.8 In health care, the terrain at our portal’s entrance holds tremendous contradiction. We hear both the eerie hush of community clinics quieted by decreased patient visits and staff furloughs and the clamor of frenzied intensive care units operating near capacity. We hear health system leaders denouncing racism while workers and patients in those systems decry racial hierarchy in day-to-day practices. We witness people experiencing homelessness being evicted from encampments while public health officials preach sheltering at home and social distancing to prevent COVID-19 infection.
Passage into a portal offers the chance to strengthen the pulsations of reimagination and re-creation. In this moment, we can listen more clearly and more closely both to ourselves and to social context. When we do so, it becomes evident that distance from social context doesn’t free us from harmful social systems and structures—proximity does. We will see that if we desire to care with compassion, heal holistically, and advance health equity, we must at times set down the stethoscope.
References
-
Foucault M. The Birth of the Clinic: An Archaeology of Medical Perception. Vintage Books; 1994.
-
Braun L. Breathing Race Into the Machine: The Surprising Career of the Spirometer From Plantation to Genetics. University of Minnesota Press; 2014.
- Berlin A, Koski-Karell V, Page KR, Polk S. The right and left hands of the state: two patients at risk of deportation. N Engl J Med. 2019;381(3):197-201.
-
Menakem R. My Grandmother’s Hands: Racialized Trauma and the Pathway to Mending Our Hearts and Bodies. Central Recovery Press; 2017.
-
Menakem R. What somatic abolitionism is. Resmaa.com. Accessed February 9, 2020. https://www.resmaa.com/movement
-
Dwamena A. Why African-American doctors are choosing to study medicine in Cuba. New Yorker. June 6, 2018. Accessed June 23, 2020. https://www.newyorker.com/science/elements/why-african-american-doctors-are-choosing-to-study-medicine-in-cuba
-
Condo J, Mugeni C, Naughton B, et al. Rwanda’s evolving community health worker system: a qualitative assessment of client and provider perspectives. Hum Resour Health. 2014;12:71.
-
Roy A. The pandemic is a portal. Financial Times. April 3, 2020. Accessed June 21, 2021. https://www.ft.com/content/10d8f5e8-74eb-11ea-95fe-fcd274e920ca