The Indian Health Service (IHS) is a federal agency within the US Department of Health and Human Services (HHS) whose mission is to raise the health status of American Indian and Alaska Native (AI/AN) people to the highest level [1]. The IHS carries out this mission through a nationwide network of hospitals and clinics in 35 states, partially funded by an annual federal appropriation of approximately $4.4 billion [2]. A significant proportion of operating budgets for IHS facilities also comes from third-party revenue collections for services delivered to patients covered by insurance.
Historically, the IHS was an entirely federal system, but in recent decades it has evolved in a profound way. Tribal governments now directly manage more than half of IHS-appropriated funds and the great majority of physical facilities under self-governance contracts and compacts. In addition, 34 nonprofit Urban Indian Health centers provide care for AI/AN people and other underserved communities in urban locations. The IHS, Tribal, and Urban (I/T/U) health care facilities have come to be known collectively the Indian health system.
IHS and tribal health care facilities are overwhelmingly located in rural and isolated settings with little access to specialty services. Travel costs to bring patients to specialists, or vice versa, in locations such as the northern plains, desert southwest, and Alaska are prohibitive. Telemedicine is therefore an ideal if not essential component of care delivery if the IHS is to accomplish its mission in these locations. While the Indian health system does not have a single, nationally coordinated telemedicine program, telemedicine is widely used. The specific needs and solutions vary from location to location, depending on population characteristics and the availability of specialty services.
Many specialties serving American Indian and Alaska Native communities use the expanding telehealth “toolkit.” One of those specialties, cardiology, has begun to build new service models using telehealth. In recent years, cardiology consultations and services have been delivered across distance and time, with interpretation of echocardiograms, electrocardiograms, and other standard cardiac tests performed by specialists at distant referral sites. The specialists hundreds or thousands of miles away thus are able to connect virtually with team members skilled at image and information acquisition who live locally or travel across a tribal nation or region.
There are even examples of care management programs in which patients’ vital signs, weight, and pulse oximetry are securely monitored via smartphones by a team trained in pattern recognition and readily available for real-time telephone consultation. Such programs in cardiac care management (e.g., the “Care Beyond Walls and Wires” program in northern Arizona) have demonstrated impressive results. Patients with timely access to expertise and care advice have improved outcomes, report greater satisfaction, and experience fewer hospitalizations and emergency department visits [3].
As telecommunication networks expand in both reach and capacity in rural communities across the United States, more patients and families are able to benefit from services when and how they need them. Many adult and pediatric specialty services are also available for Native communities through advanced telehealth tools and capability. Telehealth is increasingly important in helping I/T/U health facilities and programs close gaps in health condition recognition, diagnosis, and treatment that have existed for decades between many AI/AN communities and other communities in the United States. The sections that follow describe three broad and highly successful telehealth initiatives in Indian country and touch on some of the issues and opportunities for the future.
Telehealth in Alaska—The Alaska Federal Health Care Access Network
The Alaska Tribal Health System (ATHS) has relied on telehealth programs to deliver care to some of the most remote places in the United States for more than 20 years [4]. The largest of these programs is the Alaska Federal Health Care Access Network (AFHCAN), which has been in operation since 2001 and has been installed in 250 sites throughout Alaska. Most of these sites (180, or 72 percent) are clinics staffed by community health aides/practitioners (CHA/P) in small villages with an average population of less than 300 residents [5]. This system was originally implemented when broadband connectivity was unavailable or intermittent at most village clinics. Consequently, AFHCAN pioneered many concepts in multiorganizational “store-and-forward” telehealth (i.e., capturing images and other patient data for transmission and consultation later at a distant site) and developed technologies that are now used on all continents except Antarctica (AFHCAN Global Telehealth Solutions, LLC, unpublished data, 2014). In 2013, 1,686 clinicians in the ATHS used the AFHCAN system to deliver 36,229 episodes of care for 22,982 patients (Alaska Native Tribal Health Consortium [ANTHC], unpublished data); approximately 16 percent of all Alaska Natives were involved in telehealth in a single year (ANTHC, unpublished data).
Outcomes. The AFHCAN system has greatly improved access to care for Alaska Natives. A study conducted in Nome, for example, found that, prior to use of telemedicine for audiology and ear, nose, and throat (ENT) services, 47 percent of new patients would wait five months or longer for an in-person ENT appointment. After the introduction of telemedicine, this rate dropped to 8 percent of all patients in the first three years, and less than 3 percent of all patients in the next three years [6]. Using this service reduces patient wait times and opens up in-person appointment slots. Patients who need additional testing or in-person evaluation and care are seen in an expedited manner. In fact, most specialty consultations are now completed within two to four hours (ANTHC, unpublished data). More than 70 percent of all consultations are conducted without requiring the patient to travel to the specialist, resulting in an estimated $8 to $10-million savings annually in the state’s patient travel costs [7].
This telehealth system is now used to provide traveling mid-level practitioners access to specialist doctors [8] and enable presurgery planning [9] and postsurgery follow-up [10] for patients, leading to efficiencies and more timely access to care. AFHCAN also developed technologies to support these clinical services and now runs the only federally funded National Telehealth Technology Assessment Center (NTTAC) [11].
Contributors to adoption. The key driver for telehealth adoption in Alaska has been the commitment of more than 30 autonomous organizations in the ATHS to embrace telehealth as a strategy for improving access to care. Telehealth is a critical component of the corporate strategic plan for many organizations, and leading organizations have developed policies that mandate telehealth in certain circumstances. While the original AFHCAN program and equipment were federally funded, the ongoing costs for equipment, supplies, staffing, training, and connectivity have been borne by the participating organizations and offset by insurance reimbursement since 2001. Alaska, unlike some other states, also has a supportive environment for telemedicine adoption: the Medicaid program has reimbursed for video teleconference (VtC) and store-and-forward telehealth since 2001 [12], its “telemedicine coverage under the Medicaid plan is broad and the least restrictive compared to other states” [13], and the vast majority of third-party payers also reimburse (ANTHC, unpublished data).
The Universal Services Fund (USF) subsidy program has also contributed significantly to the growth of telehealth in Alaska. This program dramatically lowers connectivity costs for remote sites, resulting in greater bandwidth and more reliable connectivity that makes videoconferencing possible and provides greater store-and-forward capability. Currently, many tribal health organizations use VtC to deliver primary care services to rural villages (ANTHC, unpublished data). A few have expanded VtC services to provide behavioral health and physical therapy services (ANTHC, unpublished data). The ANTHC has built a high-availability, multi-organizational desktop VtC solution that is being deployed across the entire ATHS for specialties such as cardiology, oncology, endocrinology, speech-language pathology, pediatric endocrinology, pulmonology, infectious diseases, and adolescent medicine. ANTHC is also working toward the provision of live emergency teleconsultations for pediatrics, trauma, and other on-call specialty services. Preventing emergency travel or medevacs will lead to a substantially greater cost savings since “medevac ambulatory services are expensive [and] may, at times, exceed a cost of $100,000 and can cause significant financial hardship for Alaskans paying out-of-pocket for this service” [14].
The future. Telehealth in Alaska is expected to change dramatically in the coming years. The ATHS relies on 28 distinct electronic health record (EHR) systems that are now beginning to be connected to the statewide health information exchange (ANTHC, unpublished data). Providing unparalleled statewide access to clinical information will support both telemedicine and systems approaches to health care, including but not limited to population health, data analytics, and statewide lab order/entry. Almost all of these EHRs will support direct secure messaging (DSM) for the exchange of health care data and be capable of exchanging clinical documents in a consolidated clinical document architecture (CCDA) format, which makes use of templates. The integration of image capture with these EHRs will essentially turn every EHR into a store-and-forward telehealth system, vastly improve consultation and referral processes that are integrated with the EHR, and thereby upgrade the scheduling and billing systems. Finally, integration of video teleconferencing into the EHR will ease scheduling challenges and eventually permit patient-to-doctor video visits (“eVisits”).
Mobile platforms will also play a significant role in health care in the very near future. AFHCAN telehealth apps are now available on iPads, iPhones, and Android-based systems, permitting rural clinicians to capture images and create cases on mobile devices. The IHS has also funded a program to convert the 16-pound Community Health Aide Manual (CHAM) for care in village clinics into an electronic version (eCHAM) that can also be downloaded to mobile devices. The statewide desktop video teleconferencing solution is also available on these devices, and some of the EHRs will migrate to mobile devices as well. This change will allow remote clinicians to use a single mobile device for all forms of telehealth, EHR, and access to knowledge and best practices.
Telebehavioral Health: Bringing Mental Health Services to the Patient
There are significant health and health care disparities between Native populations and other groups [15], including tremendous underfunding of services in tribal communities [16]. The suicide rate among AI/ANs is 50 percent higher than the rate for white Americans [17]. This disparity is most pronounced in rural and remote areas. Additionally, many AI/AN people continue to struggle with substance use disorders [18]. On the other hand, many Native Americans have an especially strong sense of community connectedness, cultural identity, and family and social support, which are all protective factors for wellness and sobriety [19].
Although the need is extreme, especially in remote areas, access to behavioral health services is often quite limited in Native communities [20]. This is particularly true of specialty care (e.g., child psychology, addictions psychiatry). Attracting and retaining behavioral health professionals in rural or remote areas is a significant challenge. They are typically in short supply in any community and have numerous employment opportunities in urban, higher-paying, and more desirable locations. The telehealth model allows behavioral health professionals to live where they like and still provide services equivalent to in-person care to high-need, remote communities [21].
The IHS Tele-Behavioral Health Center of Excellence (TBHCE) was established in 2008 to provide behavioral health services across the country through real-time (synchronous) televideo connections. This type of service requires dedicated bandwidth; otherwise the session can be disrupted. Due to the rural, remote nature of many Native communities, Internet connectivity is often lacking or of poor quality. To overcome this barrier, these services are provided within IHS or tribal health care facilities that have faster, more stable Internet connections than patients’ homes.
Outcomes. Telebehavioral health improves continuation rates. Within the clinical telebehavioral health program we have noted that patients are 2.5 times more likely to keep their telepsychiatry appointments than in-person psychiatry sessions (TBHCE, unpublished data, 2012). This is particularly surprising, given that they have to travel to the clinic regardless of the type of session. When asked about this, the vast majority of patients said they felt that the telepsychiatry session was more confidential than an in-person session. They knew that they would not run into their therapists at the local school or grocery store and therefore felt that the risks to their confidentiality were reduced. Although the telecounseling component (i.e., providing real-time counseling services via televideo) of TBHCE is relatively new, there is also strong anecdotal evidence supporting its facilitation of the therapeutic relationship. For example, during the first two weeks of the program the psychologist was told by three different women, “if you were in the room I wouldn’t tell you this” (personal communication with program psychologist). All three then went on to disclose information the psychologist considered to be extremely relevant to their treatment.
Given that the Native population is among the most impoverished in the United States [22], it is important to consider the benefits of TBHCE for Native patients. In fiscal year 2013 the telebehavioral health program allowed IHS patients to avoid more than 500,000 miles of travel, which translated into over $305,000 in savings for them (TBHCE unpublished data). We estimate that, because the telebehavioral health program was available to patients in 2013, these patients saved more than 16,450 hours of work or school that would otherwise have been missed to travel for appointments (TBHCE, unpublished data).
Teleophthalmology: Preventing Blindness in Diabetic Patients
Diabetic retinopathy (DR) is the leading cause of new blindness among working-age adults (20-74) [23], even though serious vision loss from DR can be very nearly eliminated by timely diagnosis and treatment. The standard of care that prevents needless vision loss due to DR has been widely accepted and promulgated for four decades, but these high rates of DR persist, largely because only half of those with diabetes obtain an annual retinal examination [24]. The annual DR exam rate is similar for AI/AN patients served by the IHS, a population with extraordinarily high prevalence rates of diabetes [25].
A lack of annual DR examinations is incompletely explained by simple access-to-care factors in Indian country and probably elsewhere. The persistent failure to achieve screening targets through eye clinic-based DR examinations led the IHS to implement telemedicine in the primary care setting to improve compliance with DR standard-of-care guidelines and to decrease vision loss due to DR.
The Joslin Vision Network (JVN) is a teleophthalmology modality developed by the Joslin Diabetes Center that has been validated as equal to or better than a live, dilated retinal examination for diagnosing the level of DR and diabetic macular edema (DME) [26, 27] and is also able to identify other common non-DR eye diseases [28]. This technology does not use pupil dilation and is noninvasive, so it can be implemented in a primary care setting and easily integrated into the normal clinical workflow of care for patients with diabetes. Nearly 100 percent of the known population with diabetes could access this technology, whereas only about 50 percent of Americans with diabetes visit eye clinics [24].
Outcomes. The IHS began implementation of the JVN in Indian country in 2000 as a pilot program at two sites in Arizona. Since then the IHS-JVN Teleophthalmology Program (IHS-JVN) has grown to 92 I/T/U sites in 25 states, with more than 16,000 exams performed annually and more than 90,000 cumulative exams to date (figure 1).
Figure 1. Annual and Cumulative IHS-JVN Exams, 2000-2013 (IHS-JVN Teleophthalmology Program, unpublished data, 2014)
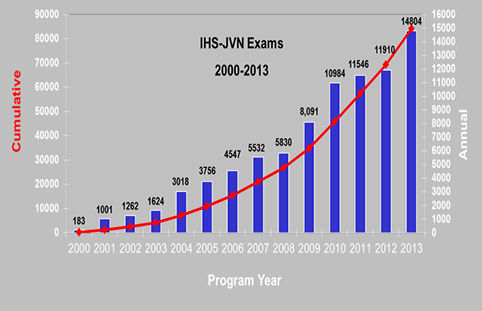
These data aid understanding of how the program works and how it can be best utilized. DR screening programs have been associated with historic improvement in DR management and clinical outcomes in large public health implementations [29], and JVN in particular has been shown effective. A 2005 study showed the IHS-JVN to be more effective and less costly than a conventional eye examination for detecting DR and preventing severe vision loss [30]. A four-year study at a large IHS facility showed that the IHS-JVN was associated with a 50 percent increase in compliance with DR standards of care [31].
Improvements in these measures throughout the enterprise have been variable, however. This variability is not completely understood but is most likely associated with staffing, program integration, and site-specific use. An additional limitation is that the current program distribution allows coverage of only 40 percent of the total AI/AN population with diabetes (IHS, unpublished data). Nonetheless, there has been an increase of almost 20 percent in the previously static IHS DR exam rate over the past seven years (49.1 percent to 58.6 percent), as IHS-JVN patient encounters have accelerated (see figure 1). This increase in the exam rate has a direct public health impact since each percentage point increase equates to approximately 100 AI/AN patients with sight-threatening DR who were identified and referred for care to prevent vision loss.
Coding and reimbursement challenges. Funding for the IHS Teleophthalmology Program has come largely through specific congressional appropriations but is supplemented by reimbursements from Medicare, Medicaid, and private insurance payers. The range of reimbursement from each varies widely but generally is insufficient for the program to break even in the short term. This is largely because Current Procedural Technology (CPT) diagnosis and treatment codes on which reimbursement is based do not accurately describe the IHS-JVN procedure, which is substantially undervalued. Appropriately valued codes that allow for a range of telemedicine services with defined clinical outcomes are needed [32]. The long-term economic value of the IHS-JVN procedure and program lies in the prevention of the costly morbidity of untreated DR, as well as in indirect savings from managing the chronic complications of diabetes in a sighted versus sight-impaired patient.
The future. Development of the IHS-JVN continues in operational, technical, and clinical areas. New software development focuses on improved interoperability to enhance clinical efficiency, patient safety, and regulatory compliance. New wide-field imaging technology will begin deployments in 2015 to further improve technical quality and diagnostic accuracy, and increased deployments of the portable IHS-JVN hardware will bring the service to more remote sites that have small populations of patients with diabetes.
For maximum benefit, this program must be integrated electronically as well as clinically. The IHS-JVN has been made interoperable with the IHS electronic medical record using Health Level-7 (HL-7), Digital Imaging and Communications in Medicine (DICOM), and Integrating the Health Care Enterprise (IHE) standards. This interoperability has facilitated operational efficiency and patient safety, and it also supports the Health Information Technology for Economic and Clinical Health (HITECH) Act’s requirements for current and future meaningful use of electronic health records.
Based upon IHS-JVN successes to date, the program has been mandated for use at all IHS hospitals and all other IHS health care facilities serving more than 500 patients with DM. Current funding and reimbursement will allow the program to extend to approximately 125 sites with coverage of approximately 60-70 percent of the AI/AN population with DM.
Evolution, Barriers, and the Future of Telehealth in Indian Country
Despite its value in reducing health disparities, the promise of telehealth has yet to be fully realized for many AI/AN people. While there are many reasons for the delayed implementation of telehealth innovation, it is the business models—the economics of health care delivery—that represent the most significant obstacle. Except for special programs within states such as Alaska, reimbursement rules and policy have lagged behind technical capability. As a result, service models in Indian health facilities that depend on reimbursement from Medicare, Medicaid, and commercial insurance are unable to capitalize on telehealth innovation because reimbursement, a critical fuel for change, is low or absent.
Efforts are underway to change reimbursement policy, supported by growing outcome data showing the quantifiable contribution of telehealth to the “triple aim” [33] of improved population health, better experiences and outcomes for patients, and reductions in cost to the community. The focus on population health may help accelerate telehealth innovation use as reimbursement policy evolves from fee-for-service to accountable care and value-based payment models. Such a change will enable telehealth tools to be incorporated into new care processes that do not rely on fee-for-service reimbursement. While this trend toward accountable care takes shape, it is vital that reimbursement policy for fee-for-service care continues to improve. Efforts must continue in both fee-for-service and accountable care payment structures for the full value of telehealth to be realized for Indian health care.
References
-
Indian Health service. Agency overview. http://www.ihs.gov/aboutihs/overview/. Accessed September 9, 2014.
-
2018;
Indian Health Service. IHS year 2014 profile. http://www.ihs.gov/newsroom/factsheets/ihsyear2014profile/. Accessed September 9, 2014.
-
Riley WT, Keberlein P, Sorenson G, et al. Program evaluation of remote heart failure monitoring: a feasibility and health care utilization analysis in a rural regional medical center [published online ahead of print July 15, 2014]. Telemed J E Health.
- Patricoski C. Alaska telemedicine: growth through collaboration. Int J Circumpolar Health. 2004;63(4):365-386.
-
Alaska Community Health Aide Program. Overview of the Alaska Community Health Aide Program. http://www.akchap.org/resources/chap_library/Referral_Physician/CHAM_CHAP_Overview.pdf. Accessed October 25, 2014.
- Hofstetter PJ, Kokesh J, Ferguson AS, Hood LJ. The impact of telehealth on wait time for ENT specialty care. Telemed J E Health. 2010;16(5):551-556.
-
Agency for Health Research and Quality. Telehealth improves access and quality of care for Alaska Natives. https://innovations.ahrq.gov/perspectives/telehealth-improves-access-and-quality-care-alaska-natives. Accessed November 25, 2014.
- Kokesh J, Ferguson AS, Patricoski C, LeMaster B. Traveling an audiologist to provide otolaryngology care using store-and-forward telemedicine. Telemed J E Health. 2009;15(8):758-763.
- Kokesh J, Ferguson AS, Patricoski C. Preoperative planning for ear surgery using store-and-forward telemedicine. Otolaryngol Head Neck Surg. 2010;143(2):253-257.
- Kokesh J, Ferguson AS, Patricoski C, et al. Digital images for postsurgical follow-up of tympanostomy tubes in remote Alaska. Otolaryngol Head Neck Surg. 2008;139(1):87-93.
- Puskin DS, Cohen Z, Ferguson AS, Krupinski E, Spaulding R. Implementation and evaluation of telehealth tools and technologies. Telemed J E Health. 2010;16(1):96-102.
-
Myers and Stauffer, LLC. Final report for Alaska Telehealth Advisory Council: Medicaid telehealth reimbursement research project. February 2002. http://dhss.alaska.gov/dph/HealthPlanning/Documents/telehealth/atac/pdfs/D4_Final.pdf. Accessed October 27, 2014.
-
Thomas L, Capistrant G. State telemedicine gaps analysis: coverage and reimbursement. Washington, DC: American Telemedicine Association; 2014. http://www.americantelemed.org/docs/default-source/policy50-state-telemedicine-gaps-analysis---coverage-and-reimbursement.pdf?sfvrsn=6. Accessed October 29, 2014.
-
Shields ME, Daniello D. Regarding: support HB 300, air ambulance services. http://dhss.alaska.gov/acoa/Documents/legislative/2014_HB300.pdf. Accessed October 25, 2014.
- Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, Forquera RA. A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. Am J Public Health. 2006;96(8):1478-1484.
- Gone JP. Mental health services for Native Americans in the 21st century United States. Prof Psychol Res Pr. 2004;35(1):10-18.
- Herne M, Bartholomew M, Weahkee RL. Suicide mortality among American Indians and Alaska Natives, 1999-2009. Am J Public Health. 2014;104(suppl 3):336-342.
-
Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/nsduhresults2011.pdf. Accessed October 15, 2014.
- Mackin J, Perkins T, Furrer C. The power of protection: a population-based comparison of native and non-native youth suicide attempters. Am Indian Alsk Native Men Health Res. 2012;19(2):20-54.
- Human J, Wasem C. Rural mental health in America. Am Psychol. 1991;46(3):232-239.
- Shore J, Savin D, Orton H, Beals J, Manson SM. Diagnostic reliability of telepsychiatry in American Indian veterans. Am J Psychiatry. 2007;164(1):115-118.
-
Pew Research Center. 1-in-4 Native Americans and Alaska Natives are living in poverty. http://www.pewresearch.org/fact-tank/2014/06/13/1-in-4-native-americans-and-alaska-natives-are-living-in-poverty/. Accessed October 25, 2014.
- Fong DS, Aiello LP, Ferris FL III, Klein R. Diabetic retinopathy. Diabetes Care. 2004;27(10):2540-2553.
-
National Committee for Quality Assurance. Improving Quality and Patient Experience: The State of Health Care Quality 2013. Washington, DC: National Committee for Quality Assurance; 2013. https://www.ncqa.org/LinkClick.aspx?fileticket=Yzvl1-QvSX0%3d&tabid=836&mid=4194. Accessed August 10, 2014.
-
Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed August 10, 2014.
-
Bursell SE, Cavallerano JD, Cavallerano AA, et al; Joslin Vision Network Research Team. Stereo non-mydriatic digital-video color retinal imaging compared with Early Treatment Diabetic Retinopathy Study seven standard field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology. 2001;108(3):572-585.
-
Cavallerano AA, Cavallerano JD, Katalinic P, et al; Joslin Vision Network Clinical Team. Use of Joslin Vision Network digital-video nonmydriatic retinal imaging to assess diabetic retinopathy in a clinical program. Retina. 2003;23(2):215-223.
- Chow SP, Aiello LM, Cavallerano JD, et al. Comparison of nonmydriatic digital retinal imaging versus dilated ophthalmic examination for nondiabetic eye disease in persons with diabetes. Ophthalmology. 2006;113(5):833-840.
-
Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 with 2009-2010. BMJ Open. 2014;4(2):e004015. http://bmjopen.bmj.com/content/4/2/e004015.full. Accessed October 30, 2014.
- Whited JD, Datta SK, Aiello LM, et al. A modeled economic analysis of a digital tele-ophthalmology system as used by three federal health care agencies for detecting proliferative diabetic retinopathy. Telemed J E Health. 2005;11(6):641-651.
- Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care. 2005;28(2):318-322.
-
Li HK, Horton M, Bursell SE, et al; American Telemedicine Association Diabetic Retinopathy Telehealth Practice Recommendations Working Group. Telehealth practice recommendations for diabetic retinopathy, second edition. Telemed J E Health. 2011;17(10):814-837.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769.