Abstract
Psychiatric aides and psychiatric technicians are part of direct care workforces in psychiatric inpatient units. They experience high rates of violence, but, compared to other members of treatment teams—including physicians, nurses, and social workers—they receive low wages. This commentary on a case considers the nature and scope of the ethical obligations of clinicians of higher social status (eg, physicians and nurses) and organizations to workers whose safety is at risk for little compensation.
Case
After high school graduation, HH hopes someday to go to college and become a health professional. For now, HH takes care of their mother, as they have for the last 3 years, and takes a 40-hour course to become a psychiatric aide. HH now works full time in an inpatient psychiatry unit, earning just above minimum wage during an overnight 8-hour shift in which they monitor a patient, who is involuntarily committed.
HH’s patient is ZZ, who is 58 years old and has a history of bipolar I disorder. ZZ’s symptoms were well controlled with risperidone and lamotrigine until a right rotator cuff repair surgery 5 days ago. Since then, ZZ has been demonstrating acute psychosis and hyperverbalism (inability to stop talking). Dr P’s and nurses’ efforts to redirect, interrupt, or calm ZZ have not succeeded, and ZZ’s agitation has now increased to aggression toward anyone who tries to administer medication.
None of the psychiatric aides wants to monitor ZZ, whose hyperverbalism is exhausting and whose aggression, when not well controlled, is unpredictable and generally feared. HH is assigned to monitor ZZ for the third night in a row. Last night was particularly stressful, as ZZ asked HH to help her use the bathroom and then pressed HH to a wall before others intervened.
In the morning, during rounds, ZZ points to a bruise on her right shoulder and shouts, “That dyke man-handled me!” Dr P, the lead psychiatrist, asks HH about the incident. Dr P looks to HH and says, “Don’t worry, we know nothing happened.”
“Nothing happened to ZZ,” HH thought, recalling yesterday when a fellow overnight psychiatric aide stated to Dr P during morning rounds that a patient had threatened her overnight. HH observed that Dr P ignored her, so HH decided not to say anything this morning about being pressed to a wall.
Commentary
Psychiatric aides and psychiatric technicians experience workplace violence at rates significantly higher than members of the general work force.1 Moreover, these workers experience violent injuries at higher rates than workers in like positions, such as nursing assistants (see Figure 1).2 A survey published by Kelly et al in 2016 examined the perceptions of well-being and safety of inpatient staff at a large public mental health hospital in California. Roughly 45% of respondents reported feeling unsafe at work, and, notably, psychiatric technicians composed 41% of the inpatient staff sampled.3
Figure 1. Nonfatal Occupational Injury and Illness Incidence Rates for Cases Involving Days Away From Work for Selective Healthcare and Protective Service Occupations by Ownership, 2017a
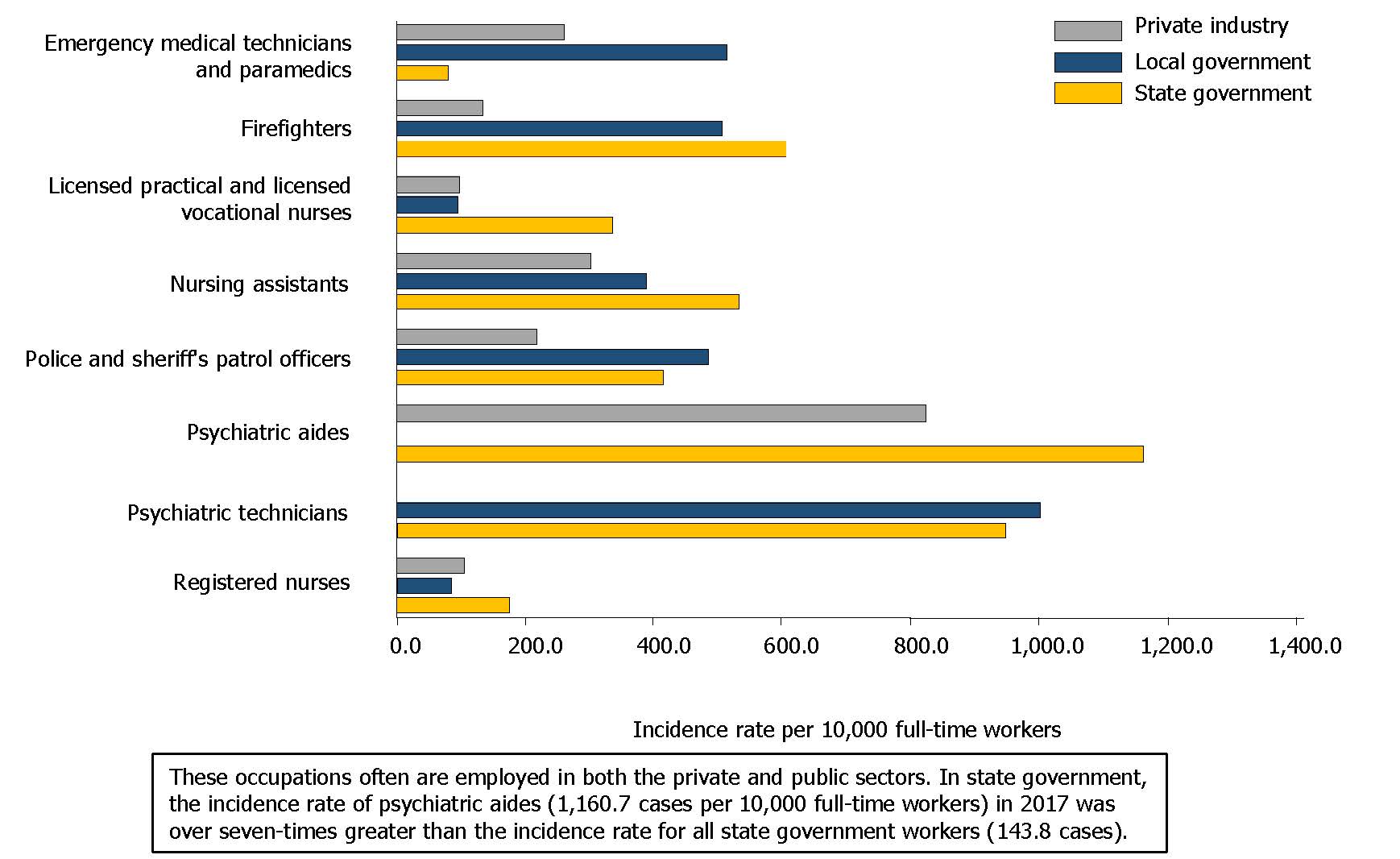
a Reproduced from US Bureau of Labor Statistics.2
In 2018, Payscale (as reported in CNN Money) listed mental health technician as one of the 15 most stressful and underpaid professions.4 The duties required of psychiatric aides and technicians are extensive, physically demanding, and hazardous. A sample description of psychiatric aides’ and technicians’ duties is presented in Figure 2.
Figure 2. Duties of Psychiatric Aides and Techniciansa
|
Psychiatric Aide Duties
Psychiatric Technician Duties
|
a US Bureau of Labor Statistics.5
Despite the demanding and hazardous nature of their work, psychiatric aides and technicians are poorly compensated and disproportionately female. In 2021, the median salary for psychiatric aides and technicians combined was $36 230 per year, or $17.42 per hour6; 73.5% of psychiatric technicians were women and 26.0% were African American.7 Educational requirements vary, but both jobs typically require a high school education, and, for technicians, a postsecondary school certificate is generally required.6 Psychiatric aides’ and technicians’ high rates of workplace violence and low pay and education levels are consistent with the finding that staff victims of psychiatric assaults tend to be younger, less formally educated, and less trained mental health workers.8
This case commentary considers barriers to employees speaking up about safety concerns and the nature and scope of the ethical obligations of higher-status clinicians (eg, physicians and nurses) and organizations to workers whose safety is at risk for little compensation.
Barriers to Communication
In this case, the psychiatrist tells HH not to worry about ZZ’s allegations, as the psychiatrist knows nothing has happened to the patient at the hands of ZZ. This interaction suggests that the problem in this patient-staff conflict is ZZ’s accusation of being “man-handled” by HH. HH’s account and experience is not solicited by Dr P, the verbal epithet cast at HH is not addressed, and the reason the psychiatrist gives no weight to ZZ’s allegations is not communicated. Given the statistics regarding the high rates of workplace violence experienced by psychiatric aides,1,2 this stance is reflective of a culture that does not protect or support them. The physical and verbal assaults experienced by direct care health care workers affect them not only physically but also psychologically by arousing feelings of helplessness, shock, anger, anxiety, frustration, and humiliation.9,10 Psychiatric unit staff who have been assaulted by patients also have an elevated risk of experiencing posttraumatic stress disorder and other mental illnesses.11
So why doesn’t HH speak up? One reason is made explicit in the case: resignation. HH’s observation that a coworker who communicated a similar experience a day earlier and was subsequently ignored left HH feeling that their voice had no ear and, therefore, there was no point in speaking up. Assessments of futility are a known reason why direct health care staff remain silent.12,13 Other reasons that staff do not speak up to team leaders such as Dr P are deeply rooted in the presence and manifestation of a long-entrenched medical hierarchy. In one survey, health care workers at lower levels of the hierarchy, such as psychiatric aides and technicians, reported speaking up about concerns less frequently than staff at higher levels of the hierarchy.13 Those of lesser prestige and power may be complying with a perceived social norm that they should stay silent.14 In addition, this norm is reinforced by those who hold authority and power.15
Thus, psychiatric aides and technicians might be afraid to speak up. This fear is linked to the concept of psychological safety. Do direct care workers feel psychologically safe to communicate concerns, ask questions, and receive and give feedback in a high-risk setting?16,17 The ability and freedom to speak up without fear of denigration or indifference helps workers at lower levels of the hierarchy navigate difficult workplace environments and thereby promotes a reduction in workplace violence and an environment of safety.18
Health Care Organizational Obligations
What are the ethical obligations of the health care organization with respect to the safety of direct care health aides and technicians? The psychiatric hospital is by nature a high-risk place. A highly reliable organization is defined as an organization with an inherent probability of hazard, such as an inpatient psychiatric unit, where the consequences of error are high but the occurrence of errors and adverse events is low.19 How is this reliability achieved?
First, the organization must have a stated commitment to the physical and psychological safety of employees.20 It must provide appropriate training to address safety and provide adequate staffing to implement a safe environment. Appropriate training, staffing, and implementation of safety procedures regarding workplace hazards does result in a reduction in the occurrence of workplace violence.21
Second, there must be an appropriate response to violent incidents, including appropriate methods for reporting and addressing violent incidents. Addressing the incident could include measures such as critical incident stress debriefing, a structured small group storytelling process combined with psychoeducation that is intended to normalize group members’ reactions to a critical incident and facilitate their recovery.22 This debriefing could be followed by counseling for individuals and reassessment of safety procedures for the organization.20 These are essential processes and have proven effective in helping employees cope with workplace violence and in reducing the consequences of violence to employees.23
Third, organizations owe workers who earn low wages inclusion in decision making. Direct care workers are the front line of observation and the front line of patient encounters. According to the Occupational Safety and Health Administration (OSHA), “A basic prerequisite for preventing injuries and illnesses is knowledge of the types, location, and underlying reasons for their occurrence in the workplace.”18 For this reason, OSHA recommends involving frontline workers in the design and implementation of policies and procedures that affect them as well as their patients.18 This type of inclusiveness minimizes the risk of harm to staff and patients alike.21,24 Conversely, direct care workers may point out that their experience of poor team communication, combined with dismissal of their experience by health care organizations, places patients and staff in danger.
Fourth, the organization owes all staff just treatment. Is there a commitment on the part of the organization to equal process—that is, are the responses of the organization to violent and adverse events suffered by doctors, nurses, social workers, therapists, aides, and technicians addressed in a like manner?25 Is there an organizational commitment to a living wage, health care, education, and promotion for all employees? Inadequate compensation is a disincentive to investment in the treatment team and can result in employees’ feelings of resignation,26,27 such as displayed by HH in the described case. Joan Acker, a well-known American sociologist, researcher, writer, and educator described inequality in organizations as follows:
I define inequality in organizations as systematic disparities between participants in power and control over goals, resources, and outcomes; workplace decisions such as how to organize work; opportunities for promotion and interesting work; security in employment and benefits; pay and other monetary rewards; respect; and pleasures in work and work relations.28
In terms of compensation, physicians and organization administrators earn salaries 4 to 7 times higher than psychiatric aides and technicians,29 who are undercompensated for the work they perform. In Texas, for example, it requires $21.98 an hour to afford a 2-bedroom rental,30 yet the average hourly wage of a psychiatric aide in Texas is $22.00 and of a technician is $27.19.31,32 In a 2019 study, Budig et al found that childcare workers, nursing aides, and health aides suffered a steep pay penalty (15% among women and 6% among men) compared to other workers of similar education, licensing, and skill.33 These disparities reflect a long history in the United States dating all the way back to slavery, a history denigrating direct care health workers based on the race and gender of these workers. The current compensation paradigm in the health care industry is the manifestation of systemic racism and misogyny within the health care industry.34
Finally, is the work culture just? A just work culture supports a psychiatric aide or technician who reports an unsafe situation or an adverse event without making that person fear reprisals from the organization.25 Such reprisals can have significant economic impact if an aide loses their employment as a result of making a report. As are psychologically safe cultures, just cultures are associated with reductions in adverse events.16,25
Psychiatrists’ Obligations as Team Leader
Olivia Ray Friedman explored interdisciplinary team functioning, coherence, and unit effectiveness in a long-term adolescent inpatient psychiatric unit in her doctoral thesis, Exploring Communication Between Staff and Clinicians on an Inpatient Adolescent Psychiatric Unit.35 Her survey study was particularly focused on capturing the perceptions of mental health counselors (eg, psychiatric aides and technicians) on team functioning and how satisfied these team members were with their level of input and involvement in team decision making. The results of her survey of 84 team members, including mental health counselors, physicians, psychologists, nurses, and social workers, indicated that one of the biggest barriers to effective function was that clinician leaders didn’t invite input from mental health counselors,35 much like Dr P did not solicit input from HH. How can clinician leaders be more inclusive?
First, Dr P, presumably as the team leader, owes all members of the direct care staff strong leadership. Strong leadership cultivates a culture of cohesiveness and effective communication; it is a characteristic of success in highly reliable organizations.36 Psychiatrists are, by education and practice, particularly skilled in building rapport, negotiating, understanding group dynamics, managing conflict, and prioritizing relationships.21 Given these skills, they can be motivational and help guide the team toward mutually recognized objectives.36 To do so, the leader must utilize the knowledge and skills of all those on rounds who are involved in patient care, including psychiatric aides and technicians, by soliciting their input, giving them voice, and supporting their position. It is notable that direct care staff appreciate the presence of psychiatrists on the floor with them in providing guidance, reassurance, and support.37
Second, psychiatrists as team leaders owe the psychiatric aides and technicians a strong response to violent incidents. Violent events decrease staff morale, increase staff turnover, and harm individuals.21,37 Team leaders owe them, just as organizations do, an acknowledgment of experienced events and a consistent method for addressing these events with the provision of assessment, comfort, and support.
Third, physicians and team leaders owe their staff justice, just as organizations do. Physicians benefit greatly within health care organizations as employees, contractors, or administrators. In not hearing HH, Dr P makes the psychiatric unit a more dangerous place and agrees, if tacitly, with a system of inequality that puts workers earning low wages at risk by taking advantage of the fact that it would be difficult for HH to walk away, given the limited economic power held by such workers.26
It is within the ethical purview of physicians to advocate for essential, direct care employees to receive dignified salaries and other benefits that cover the necessities of life and good health: safe workplaces, stable housing, transportation, food, comprehensive health insurance, paid sick leave, and prospects for career advancement.
Justice as a Conclusion
Psychiatric aides and technicians have voiced their desire for safe environments, better working conditions, better compensation, higher regard, and being part of the team.37 Organizations are ethically obligated to remove barriers to these voiced concerns by providing training and opportunities for education and tuition assistance that pave the way for career advancement.38 These interventions increase productivity, improve morale, and offer direct care workers opportunities for a better life—that is, they open up possibilities of home ownership, appropriate health care for the workers and their families, and advancement opportunities.26
Organizations and team leaders are ethically obligated to make a commitment to strong leadership and to creating and maintaining a physically and psychologically safe workspace for patients and team members. They must address the inequalities that exist within the organization between those with high prestige and those with less, and, by doing so, they will confer their regard and respect for those on the front lines of psychiatric care and make the psychiatric unit a safer place.
References
-
Longton L; US Bureau of Labor Statistics. A look at violence in the workplace against psychiatric aides and psychiatric technicians. Monthly Labor Review. March 2015. Accessed December 20, 2021. https://www.bls.gov/opub/mlr/2015/article/a-look-at-violence-in-the-workplace-against-psychiatric-aides-and-psychiatric-technicians.htm#:~:text=Psychiatric%20aides%20and%20technicians%20are,it%20is%2038%20times%20higher
-
2017 Survey of Occupational Injuries & Illnesses charts package. US Bureau of Labor Statistics. November 8, 2018. Accessed December 12, 2021. https://www.bls.gov/iif/osch0062.pdf
- Kelly EL, Fenwick K, Brekke JS, Novaco RW. Well-being and safety among inpatient psychiatric staff: the impact of conflict, assault, and stress reactivity. Adm Policy Ment Health. 2016;43(5):703-716.
-
Braverman B. Stressful jobs that pay badly: mental health technician. CNN Money. January 2, 2018. Accessed January 27, 2022. https://money.cnn.com/gallery/pf/2018/01/02/stressful-jobs-2017/8.html
-
Occupational Outlook Handbook: psychiatric technicians and aides: what psychiatric technicians and aides do. US Bureau of Labor Statistics. Accessed November 24, 2021. https://www.bls.gov/ooh/healthcare/psychiatric-technicians-and-aides.htm#tab-2
-
Occupational Outlook Handbook: psychiatric technicians and aides: summary. US Bureau of Labor Statistics. Accessed April 14, 2022. https://www.bls.gov/ooh/healthcare/psychiatric-technicians-and-aides.htm#tab-1
-
Labor force statistics from the Current Population Survey: household data annual averages 11: employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. US Bureau of Labor Statistics. Updated January 20, 2022. Accessed July 20, 2022. https://www.bls.gov/cps/cpsaat11.htm
- Flannery RB Jr, LeVitre V, Rego S, Walker AP. Characteristics of staff victims of psychiatric patient assaults: 20-year analysis of the Assaulted Staff Action Program. Psychiatr Q. 2011;82(1):11-21.
- Hellzen O, Asplund K, Sandman PO, Norberg A. The meaning of caring as described by nurses caring for a person who acts provokingly: an interview study. Scand J Caring Sci. 2004;18(1):3-11.
- Gerberich SG, Church TR, McGovern PM, et al. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses’ Study. Occup Environ Med. 2004;61(6):495-503.
-
Richter D, Berger K. Post-traumatic stress disorder following patient assaults among staff members of mental health hospitals: a prospective longitudinal study. BMC Psychiatry. 2006;6:15.
-
Schwappach DL, Gehring K. Trade-offs between voice and silence: a qualitative exploration of oncology staff’s decisions to speak up about safety concerns. BMC Health Serv Res. 2014;14:303.
- Schwappach DLB, Niederhauser A. Speaking up about patient safety in psychiatric hospitals—a cross-sectional survey study among healthcare staff. Int J Ment Health Nurs. 2019;28(6):1363-1373.
- Spencer PC, Munch S. Client violence toward social workers: the role of management in community mental health programs. Soc Work. 2003;48(4):532-544.
- Ung L, Stanford FC, Chodosh J. “All labor has dignity”—the case for wage equity for essential health care workers. N Engl J Med. 2021;385(17):1539-1542.
-
O’Donovan R, De Brún A, McAuliffe E. Healthcare professionals experience of psychological safety, voice, and silence. Front Psychol. 2021;12:626689.
- Newman A, Donohue R, Eva N. Psychological safety: a systematic review of the literature. Hum Resour Manage Rev. 2017;27(3):521-535.
-
US Department of Labor. Organizational safety culture—linking patient and worker safety. Occupational Safety and Health Administration. Accessed February 19, 2022. https://www.osha.gov/healthcare/safety-culture-full
- Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41(4, pt 2):1576-1598.
-
US Department of Labor. Guidelines for preventing workplace violence for healthcare and social service workers. OSHA 3148-06R 2016. Occupational Safety and Health Administration; 2016. Accessed December 12, 2021. https://www.osha.gov/Publications/osha3148.pdf
- d’Ettorre G, Pellicani V. Workplace violence toward mental healthcare workers employed in psychiatric wards. Saf Health Work. 2017;8(4):337-342.
-
Mitchell JT. Critical incident stress debriefing (CISD). Trauma.org. Accessed December 19, 2021. http://www.info-trauma.org/flash/media-f/mitchellCriticalIncidentStressDebriefing.pdf
- Anderson A, West SG. Violence against mental health professionals: when the treater becomes the victim. Innov Clin Neurosci. 2011;8(3):34-39.
- Shore LM, Cleveland JN, Sanchez D. Inclusive workplaces: a review and model. Hum Resour Manage Rev. 2018;28(2):176-189.
-
Mengstie MM. Perceived organizational justice and turnover intention among hospital healthcare workers. BMC Psychol. 2020;22;8(1):19.
-
Weller C, Almeida B, Cohen M, Stone R. Making care work pay: how paying at least a living wage to direct care workers could benefit care recipients, workers, and communities. LeadingAge LTSS Center @UMass Boston; 2020. Accessed December 20, 2021. https://www.ltsscenter.org/wp-content/uploads/2020/09/Making-Care-Work-Pay-Report-FINAL.pdf
-
O’Leary KJ, Sehgal NL, Terrell G, Williams MV; High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2012;7(1):48-54.
- Acker J. Inequality regimes: gender, class, and race in organizations. Gend Soc. 2006;20(4):441-464.
-
Occupational Outlook Handbook: healthcare occupations. US Bureau of Labor Statistics. Updated April 18, 2022. Accessed July 20, 2022. https://www.bls.gov/ooh/healthcare/home.htm
-
Feldman EM. Minimum wage workers struggle to pay rent in Austin more than any other Texas city, report says. Austin-American Statesman. July 16, 2021. Accessed December 20, 2021. https://www.statesman.com/story/news/2021/07/16/austin-most-expensive-city-texas-according-report-minimum-wage-rent/7967978002/
-
Psychiatric aide salary in Texas. ZipRecruiter. April 14, 2022. Accessed April 21, 2022. https://www.ziprecruiter.com/Salaries/Psychiatric-Aide-Salary--in-Texas
-
Psychiatric technician salary in Texas. Indeed.com. April 5, 2022. Accessed April 21, 2022. https://www.indeed.com/career/psychiatric-technician/salaries/TX
- Budig MJ, Hodges MJ, England P. Wages of nurturant and reproductive care workers: individual and job characteristics, occupational closure, and wage equalizing institutions. Soc Probl. 2019;66(2):294-319.
- Dill J, Duffy M. Structural racism and Black women’s employment in the US health care sector. Health Aff (Millwood). 2022;41(2):265-272.
-
Friedman O. Exploring Communication Between Staff and Clinicians on an Inpatient Adolescent Psychiatric Unit. Dissertation. Antioch University; 2021. Accessed April 12, 2022. https://aura.antioch.edu/cgi/viewcontent.cgi?article=1735&context=etds
- Gabel S. Power, leadership and transformation: the doctor’s potential for influence. Med Educ. 2012;46(12):1152-1160.
-
Totman J, Hundt GL, Wearn E, et al. Factors affecting staff morale on inpatient mental health wards in England: a qualitative investigation. BMC Psychiatry. 2011;11:68.
-
McDermott J, Goger A. The health care workforce needs higher wages and better opportunities. The Avenue blog. December 2, 2012. Accessed February 20, 2022. https://www.brookings.edu/blog/the-avenue/2020/12/02/the-heath-care-workforce-needs-higher-wages-and-better-opportunities/



