Abstract
When there is an evidence base that could be used credibly to justify expedited US Food and Drug Administration review, emergency use authorization, or approval, interventions-in-development must be evaluated in terms of their possible downstream influence on public trust and confidence in regulatory processes during a national public health crisis. When regulatory decisions express overconfidence about a prospective intervention’s success, there is risk that the costliness of or misinformation about the intervention will exacerbate health inequity. A converse risk is regulators’ underestimation of an intervention’s value in treating populations at risk for inequitable care. This article considers the nature and scope of clinicians’ roles in regulatory processes in which such risks must be considered and balanced to promote public safety and public health.
Responsible Clinician Advocacy
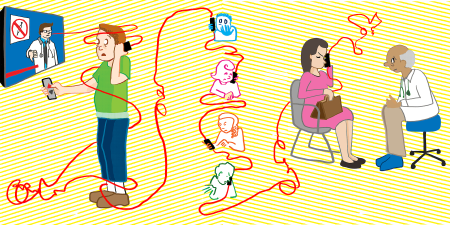
Public trust in medical treatments is an essential consideration in ethical deliberations on regulatory review, emergency use authorization, or approval of interventions-in-development. Because knowledge of the efficacy of medical treatments depends greatly on the degree to which health professionals prescribe or recommend them, as well as on whether citizens adhere to these recommendations, clinician advocacy during the regulatory process has manifold implications for health outcomes. Clinician advocacy for or against potential treatments, given a plausible evidence base that favors approval, must be considered in light of (1) a treatment’s potential implications for public confidence in regulatory processes and (2) clinicians’ judgments about whether the regulator is fairly evaluating the new product. This article examines the ethical dimensions of physician voice in the public sphere when new agents are being evaluated, authorized, or approved in a context of high uncertainty. If the decisions made during the regulatory process exhibit regulators’ overconfidence in a prospective intervention under consideration—risking inequity exacerbation due to the cost of or spread of misinformation about that prospective intervention—then physicians might weigh in against authorization or approval. Conversely, if regulators underestimate the prospective treatment value of a new product for some subpopulations, then physicians might speak publicly to draw attention to the treatment’s potential value.
Trust During the Pandemic?
The US Food and Drug Administration (FDA) has long held a high public reputation among citizens, scientists, and clinicians,1 although public trust in the FDA has recently declined.2 Previous literature has consistently shown that patient trust in clinicians remains high, in part because of the trust that many individuals have in their own doctor and the professional status of a physician,3 although trust in doctors has also declined during the pandemic.4 Clinician involvement in regulatory procedure is imperative at a time when medical regulators like the FDA are seeking to improve transparency and gain public trust, even going so far as to involve patients in the regulatory process.5
Clinicians’ engagement in the regulatory process can take multiple forms, such as their involvement in advisory or decision-making groups or in writing editorials, evidence reviews, or other forms of public commentary on the drugs or devices in question.6 The role of physicians in reporting instances of adverse outcomes or observations of negative health effects in patients they treated with interventions that have received FDA approval cannot be overstated. In this manner, physicians can provide important information for the evidence base of a particular drug or medical device through broad observation of their patient population. Ultimately, clinicians must be involved in the ethical and medical considerations pertinent to the regulation of medical products that require governmental oversight and approval, and any potential reservations they have in relation to these products should be taken very seriously.
The COVID-19 pandemic presented a significant challenge for clinical advocates pushing for vaccination uptake to mitigate the spread of the virus. Vaccine hesitancy was particularly high during the first months of the pandemic, with a large spike in hesitancy during the sixth and seventh months of the pandemic (September and October 2020), especially among Black Americans, Asian-Americans, and Native Americans,7 following significant instances of the Trump administration’s political interference in the FDA,8 which presumably contributed to public fears that authorization of the vaccine would be politically motivated. (Vaccine hesitancy did decline among people of color following the vaccine rollout, however.9,10) Figures like Anthony Fauci, then director of the National Institute of Allergy and Infectious Diseases and a member of the Trump Administration’s Coronavirus Task Force, provided significant reassurance to the public with regular national addresses regarding the safety and efficacy of the vaccine, despite the accelerated timeline for its emergency use authorization and later approval by the FDA.
Low-quality products are often more heavily advertised, and the effect of this publicity is likely to be higher for those who are less educated or who have access to lower-quality medical services.
Clinician advocacy can have downstream effects on public confidence in the product.11 The COVID-19 pandemic presented a crucial opportunity for clinicians to speak up against the emergency use authorization of drugs without substantial evidence in support of their therapeutic value. In cases of overconfidence in drugs, such as hydroxychloroquine, some physicians’ advocacy against medication unproven to treat coronavirus contrasted with other physicians’ promotion of these pharmaceuticals as a substitute for vaccination.12 In one such case, immense pressure by the Trump Administration on the FDA in the early stages of the pandemic led to emergency use authorization for hydroxychloroquine to treat coronavirus.13 Clinician governors, such as Fauci and other former public health officials, spoke up against the FDA decision.13,14 The FDA later reversed its emergency use authorization for hydroxychloroquine, especially in light of the severe cardiac events associated with the drug.15 While cause-and-effect is impossible to establish, it is quite possible that clinician advocacy in the case of hydroxychloroquine reduced its use and contributed to the eventual reconsideration and reversal of its authorization.16
Countering Therapeutic Overconfidence
Clinician criticism of particular therapeutic agents is important to prevent these agents’ use exacerbating inequalities. When agents are authorized for emergency use based on thin evidence or when procedural irregularities have affected a decision, disadvantaged populations might be differentially affected for several reasons. First, low-quality products are often more heavily advertised,17 and the effect of this publicity is likely to be higher for those who are less educated or who have access to lower-quality medical services. It is for this reason that independent physician advice—when coordinated with established, sound guidelines—may help protect marginalized populations from suboptimal prescription and usage patterns. Second, members of marginalized populations might be more distrustful of government and scientific institutions,18 and this distrust can spill over to contemporary care settings. In these cases, physician independence (especially as perceived by marginalized populations) could help increase badly needed trust in therapeutics.19
It is furthermore important to consider the basis of clinician-advocates’ judgments regarding whether the regulator is properly evaluating the new product or not. An example of physicians providing a vital counterweight to regulatory overconfidence is FDA approval of aducanumab. After regulatory approval of this drug in spite of an expert panel voting against approval—with 10 members voting against and 1 voting “uncertain”—the public voice of clinicians who disagreed with the decision of regulators was significant in bringing attention to the decision.20 Following the FDA approval of the drug over the clear and unanimous advice of the relevant scientific advisory committee, clinicians spoke up in 2 ways. First, individuals such as Aaron Kesselheim of Harvard Medical School, Mayo Clinic neurologist David Knopman, and Washington University neurologist Joel Perlmutter, publicly resigned from their positions as members of a primary advisory committee to the FDA.21 Second, leading hospitals, such as Cleveland Clinic and Mount Sinai, made public announcements that their physicians would not be prescribing aducanumab.22 The decision of these clinician experts to speak up against the agency was particularly significant, as it called into question the FDA’s trustworthiness in the process of drug approvals. Although physician protest may further erode trust in regulatory agencies in the short run, physician advocacy in favor of scientific rigor presents an important opportunity to engage the public in understanding the validity of the drug approval process and the importance of rigorous scientific evaluation of new agents.
Circumspect Courage
The advocacy work of clinicians in contexts such as these must be considered carefully. Idiosyncratic reliance upon personal opinions is never a sound basis for clinical advice, prescribing patterns, or medical treatment. Assuming a plausible evidence base that justifies authorization or approval, clinical criticism or suspicion must be considered in light of 2 variables. The first is the potential implications of clinical statements or advocacy for downstream public confidence in therapeutics. The key here is public confidence not in any therapeutics but in the right therapeutics—namely, those whose use is proven to improve health outcomes and that will, in addition, potentially reduce health inequities. The second variable concerns judgments about whether the regulator is properly evaluating a new product. If regulatory decisions express overconfidence in a prospective intervention—as might have occurred during review of aducanumab or for emergency use authorization of hydroxychloroquine or convalescent plasma—then expected usage patterns might worsen health inequity without raising population health due to the high cost of the drug (aducanumab) or to misinformation about the drug (hydroxychloroquine) affecting certain groups more than others. In such cases, independent physician criticism of the evidence base for prospective interventions might be appropriate for countering regulatory overconfidence. If regulators underestimate a prospective intervention’s value for subpopulations, on the other hand, then physicians might call attention to that intervention’s possible value to some underserved populations.
References
-
Carpenter D. Reputation and Power: Organizational Image and Pharmaceutical Regulation at the FDA. Princeton University Press; 2010.
-
Simmons-Duffin S. Poll finds public health has a trust problem. NPR. May 13, 2021. Accessed October 21, 2022. https://www.npr.org/2021/05/13/996331692/poll-finds-public-health-has-a-trust-problem
-
Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2003;79(4):613-639.
-
ABIM Foundation. Surveys of trust in the US health care system. NORC; 2021. Accessed October 21, 2022. https://buildingtrust.org/wp-content/uploads/2021/05/20210520_NORC_ABIM_Foundation_Trust-in-Healthcare_Part-1.pdf
-
Carpenter D, Kesselheim AS, Joffe S. Reputation and precedent in the Bevacizumab decision. N Engl J Med. 2011;365(2):e3.
-
FDA-led Patient-Focused Drug Development (PFDD) public meetings. US Food and Drug Administration. July 18, 2022. Accessed August 22, 2022. https://www.fda.gov/industry/prescription-drug-user-fee-amendments/fda-led-patient-focused-drug-development-pfdd-public-meetings
-
Bhaskar A. Understanding Trust in the Food and Drug Administration and the Centers for Disease Control During the Coronavirus Pandemic: Analyzing Survey Data to Characterize Demographic Differences in Trust and the Relationship between Trust and Political Interference. Bachelor’s thesis. Harvard College; 2022.
-
Karlin-Smith S. Plasma authorization raises fears of politically-influenced COVID-19 vaccine decisions, compromised FDA. Pharma Intelligence. Accessed August 24, 2020. https://pharmaintelligence.informa.com/resources/product-content/plasma-authorization-raises-fears-of-politically-influenced-covid19-vaccine-decisions-compromised-
-
Padamsee TJ, Bond RM, Dixon GN, et al. Changes in COVID-19 vaccine hesitancy among Black and White individuals in the US. JAMA Netw Open. 2022;5(1):e2144470.
- Daly M, Jones A, Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to March 29, 2021. JAMA. 2021;325(23):2397-2399.
- Carpenter C, Grimmer J, Lomazoff E. Approval regulation and endogenous consumer confidence: theory and analogies to licensing, safety, and financial regulation. Regul Gov. 2010;4(4):383-407.
- Rubin R. When physicians spread unscientific information about COVID-19. JAMA. 2022;327(10):904-906.
-
Select Subcommittee on the Coronavirus Crisis. A “knife fight” with the FDA: the Trump White House’s relentless attacks on the FDA’s coronavirus response. US House of Representatives; 2022. Accessed November 1, 2022. https://coronavirus.house.gov/sites/democrats.coronavirus.house.gov/files/2022.08.24%20The%20Trump%20White%20House%E2%80%99s%20Relentless%20Attacks%20on%20FDA%E2%80%99s%20Coronavirus%20Response.pdf
-
Piller C. Former FDA leaders decry emergency authorization of malaria drugs for coronavirus. Science. April 7, 2020. Accessed November 1, 2022. https://www.science.org/content/article/former-fda-leaders-decry-emergency-authorization-malaria-drugs-coronavirus
-
Thomas K. FDA revokes emergency approval of malaria drugs promoted by Trump. New York Times. June 15, 2020. Updated October 6, 2021. Accessed August 22, 2022. https://www.nytimes.com/2020/06/15/health/fda-hydroxychloroquine-malaria.html
-
Frequently asked questions on the emergency use authorization (EUA) for chloroquine phosphate and hydroxychloroquine sulfate for certain hospitalized COVID-19 patients. US Food and Drug Administration. June 15, 2020. Accessed July 21, 2022. https://www.fda.gov/media/136784/download
- Parker PM. “Sweet lemons”: illusory quality, self-deceivers, advertising, and price. J Mark Res. 1995;32(3):291-307.
-
Huang Y, Green MC. Reducing COVID-19 vaccine hesitancy among African Americans: the effects of narratives, character’s self-persuasion, and trust in science. J Behav Med. Published online March 19, 2022.
- Bogart LM, Ojikutu BO, Keshav T, et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among Black Americans living with HIV. J Acquir Immune Defic Syndr. 2021;86(2):200-207.
-
Bell J, Gardner J, Pagliarulo N. FDA advisers vote against Biogen’s Alzheimer’s drug, leaving its future in doubt. BioPharma Dive. November 6, 2020. Updated November 7, 2020. Accessed July 21, 2022. https://www.biopharmadive.com/news/fda-advisory-panel-vote-biogen-alzheimers-aducanumab/588580/
-
Lovelace B Jr. Third member of prestigious FDA panel resigns over approval of Biogen’s Alzheimer’s drug. CNBC. June 10, 2021. Accessed July 21, 2022. https://www.cnbc.com/2021/06/10/third-member-of-prestigious-fda-panel-resigns-over-approval-of-biogens-alzheimers-drug.html
-
Belluck P. Cleveland Clinic and Mount Sinai won’t administer Aduhelm to patients. Center for Genetics and Society. July 14, 2021. Accessed August 22, 2022. https://www.geneticsandsociety.org/article/cleveland-clinic-and-mount-sinai-wont-administer-aduhelm-patients