Abstract
Qualitative data can supplement and contextualize quantitative data and can be useful in disability determinations to help clinicians gain fuller understanding of patients’ experiences of chronic illness or disability. This commentary response to a case suggests the importance for patient-centered care of physicians guiding patients’ documentation of their own illness experiences. Specifically, patients writing daily journal briefs about work-related activities and pain can help clinicians offer recommendations, facilitate disability determination processes, and motivate employers’ understandings of reasonable accommodations.
Case
CR is a 52-year-old woman who suffered a concussion in a car accident. CR struck the left side of her frontal bone against the car’s dashboard and was transported by ambulance to a hospital. Computed tomography and magnetic resonance imaging ruled out hemorrhage, and imaging studies were negative. CR was scheduled for an outpatient visit with a local neurologist, Dr N, and was sent home with symptoms of headache, photophobia, nausea, and fatigue, which persisted. CR reported to Dr N about 1 week after the accident that she felt “hazy” and was crying a lot. Dr N encouraged CR to try to avoid stress, screens, and sensory overstimulation. CR used up her 2 weeks of vacation time to recover.
Now 1 year after the accident, CR’s postconcussive symptoms1,2 are ongoing. She reports to Dr T, her primary care physician, that she’s frustrated about not feeling able to return to work full time and to daily activities with family. She reports feeling guilty for resting, but sounds and light still frequently trigger disabling nausea and headaches. CR knows she needs time to heal, but she is concerned about losing her job, falling short on mortgage payments, and providing for her family. One problem is that CR’s job requires nearly constant screen interaction, which also triggers debilitating symptoms. CR states that her manager has asked her to “step it up” and adds, “I look fine, so people don’t understand what I am going through and are frustrated when it takes me so long to do things I used to do quickly.”
CR presents disability benefits forms to Dr T and asks for help completing these forms. Without reliable serological tests or imaging studies to quantify CR’s symptoms’ severity or help determine her prognosis, Dr T consults Dr N. Both physicians are unsure about whether postconcussive syndrome1,2 is a qualifying disability. They wonder how to respond to CR’s request for help with the forms.
Commentary
Chronic illnesses and diseases that are rare, difficult to see, or have effects that are difficult to quantify can be challenging to treat and diagnose. Variability in symptom presentation and in illnesses’ clinical definitions further complicate different stakeholders’ understandings of chronic illnesses. These illnesses present additional challenges when clinicians try to assess the nature and scope of a disability or to facilitate patients’ acquisition of reasonable accommodations, which also vary by disability and by organizational programs or policies. In this case, the physicians must consider gaps in their own knowledge of CR’s chronic illness in order to collect information needed to complete CR’s forms. Patient-centered techniques, such as journaling, with guidance from Dr T, could help CR document with specificity how her illness impedes her performance of job-specific tasks. Journaling would also likely help Dr T care well for CR.
Qualifying for Disability Benefits
The 1990 Americans with Disabilities Act (ADA) defines an individual’s disability as “a physical or mental impairment that substantially limits one or more major life activities.”3 Impairments can include a variety of symptoms or illnesses, including those that are difficult to quantify or measure, but the ADA does not set criteria. Does postconcussion syndrome fit this definition of disability?
Fear of discrimination, job loss, promotion ineligibility, or marginalization can also prevent patients from disclosing a disability to an employer.
Concussions, which are “trauma-induced brain dysfunction,” have multiple credible definitions,4 so matching clinical indicators with disability designations illuminate 2 key areas of difficulty: definition agreement and short- and long-term symptom recognition and diagnosis. An additional challenge is how gender and racial/ethnic inequity, exacerbated by lack of diversity in research samples, should be addressed in disability assessment and documentation. In stroke research, for example, women of color are understudied when compared with White men, White women, and men of color.5 Recent concussion research has focused even more specifically on men with sports injuries.4
Additionally, clinical discernment of long-term chronic illnesses’ effects is difficult when patients develop chronic illnesses after initially trying to hide their job-specific impairment at work. This coping strategy might reflect some patients’ struggle to integrate their disability into their professional identity. Gender and cultural background can also influence how people manage and express pain.6 Fear of discrimination, job loss, promotion ineligibility,7 or marginalization can also prevent patients from disclosing a disability to an employer. Journaling could help CR clarify for Dr T how she meets criteria for accommodations or disability benefits.
Support Planning
Facilitating CR’s journaling could help CR develop a self-advocacy and self-care skill set,8 as well as provide Drs N and T with additional information needed for disability assessment. Tag-it-Yourself, for example, is a digital application that helps patients with diabetes document changes in their blood glucose levels and those changes’ relationships with their experiences of daily activities.8 CR and Dr T can work together to create a focused journal for CR to log postconcussion syndrome experiences that could help Dr T complete needed forms and develop a patient-centered care plan.
At first, journaling can feel daunting to patients already exhausted by pain and disability, but it can be critical for adding specificity to assessments of “essential” job function performance capacity, which is a key component of the definition of a “qualified individual with a disability” on the ADA “Questions and Answers” page:
A qualified individual with a disability is a person who meets legitimate skill, experience, education, or other requirements of an employment position that s/he holds or seeks, and who can perform the essential functions of the position with or without reasonable accommodation. Requiring the ability to perform “essential” functions assures that an individual with a disability will not be considered unqualified simply because of inability to perform marginal or incidental job functions. If the individual is qualified to perform essential job functions except for limitations caused by a disability, the employer must consider whether the individual could perform these functions with a reasonable accommodation. If a written job description has been prepared in advance of advertising or interviewing applicants for a job, this will be considered as evidence, although not conclusive evidence, of the essential functions of the job.9
Since the ADA “Questions and Answers” page considers a written job description as evidence of essential job functions, obtaining one could be a good place to start. If there is no formal written description of her current job, CR could work with her supervisor to create a list of essential job functions, such as data entry requiring a substantive amount of sedentary time in front of a computer. CR could then document her efforts to perform and difficulties in performing these functions, which would also let her employer know that she is actively working to complete her work-related tasks. To help CR record types and intensity of activity-specific pain (eg, headache), Drs T and N could recommend that CR note an activity (eg, computer use) or environment (eg, lighting, noise) that causes pain, indicate an associated pain intensity from 0 to 10 (eg, 0 = no pain, 5 = moderate pain, 10 = worst pain), and indicate which actions help mitigate pain. CR could enter such information several times throughout the day. The Wong-Baker FACES quickly enables the matching of a specific moment or activity to a pain level (see Figure).10 Both successful and unsuccessful actions should be noted to help CR give Drs T and N more context for understanding the nature and scope of her task-specific impairments.
Figure. Wong-Baker FACES® Pain Rating Scale
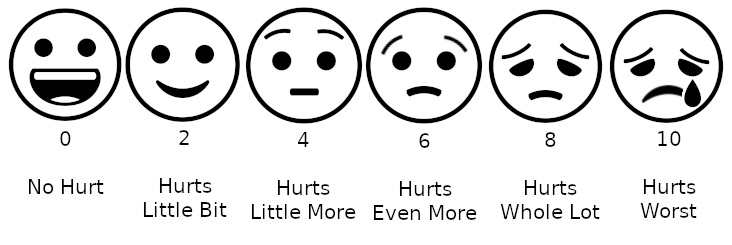
Image by Lord Belbury. Licensed under Creative Commons Attribution-Share Alike 4.0 International.
Conclusion
Focused journaling can help CR cultivate self-care and self-advocacy skills and can also help Drs T and N motivate CR’s care plan and access to reasonable accommodations and benefits from employers or government agencies. Journaling generates qualitative data and offers another tool that patients and clinicians can draw upon to manage chronic illnesses and their effects on patients’ social, home, and work lives.
References
- Ryan LM, Warden DL. Post concussion syndrome. Int Rev Psychiatry. 2003;15(4):310-316.
-
Dwyer B, Katz DI. Postconcussion syndrome. Handb Clin Neurol. 2018;158:163-178.
-
Americans With Disabilities Act of 1990, as amended, 42 USC 126, §12102 (2009).
-
Meehan WP III. Concussions. Greenwood; 2016.
- Boehme AK, Siegler JE, Mullen MT, et al. Racial and gender differences in stroke severity, outcomes, and treatment in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23(4):e255-e261.
-
Glenn CL. Reframing personal and professional identity in connection to “ability.” In: Morant Williams K, Morant FS, eds. Reifying Women’s Experiences With Invisible Illness: Illusions, Delusions, Reality. Lexington Books; 2017:81-93.
-
Wilkinson W, Frieden L. Glass-ceiling issues in employment of people with disabilities. In: Blanck PD, ed. Employment, Disability, and the Americans With Disabilities Act: Issues in Law, Public Policy, and Research. Northwestern University Press; 1999:68-102.
-
Storni C. Design challenges for ubiquitous and personal computing in chronic disease care and patient empowerment: a case study rethinking diabetes self-monitoring. Pers Ubiquit Comput. 2014;18:1277-1290.
-
Americans With Disabilities Act questions and answers. Ada.gov. Updated December 29, 2005. Accessed February 10, 2021. https://www.ada.gov/employmt.htm
-
Wong-Baker FACES Foundation website. Accessed August 3, 2020. https://wongbakerfaces.org/