In the 20th and 21st centuries, human immunodeficiency virus (HIV), severe acute respiratory syndrome (SARS), and the threat of bioterror attacks have raised questions about the role of the physician in response to epidemics. Modern medical ethics, with its precepts of beneficence, nonmaleficence, and respect for patient autonomy, focuses almost exclusively on the relationship between the doctor and patient. As a result, this ethical framework is less well-equipped to deal with the relationship of the physician to society as a whole. Personal autonomy is often at odds with public health ethics, which stress the needs of the population over the needs of the individual.
The emphasis on the personal over the public applies to physicians as well as to their patients. Indeed, in the face of modern epidemics, the concept of a “duty-to-treat”—although explicitly and forcefully stated in the professional codes of the 19th and early 20th centuries—has been in conflict with a physician’s autonomy in determining whom he or she will treat [1].
While the ethical challenges of today may be new, the threat of epidemic is not. It was present when, in 1354, Henry, first Duke of Lancaster and grandfather of Henry IV, began writing a devotional treatise. Composed of daily entries, Le Livre de Seyntz Medicines (The Book of Holy Medicine) is unique among medieval devotional literature in that it contains the most extensive known use of medical metaphors and imagery to describe religious experience. The book is a catalogue of Henry’s sins, expressed as various wounds and diseases, followed by a similar account of spiritual remedies in the form of common medieval medical treatments [2]. What ultimately moved Henry to write this work remains a mystery, but coming so soon after the first arrival of the Black Death in England in 1347, it is not hard to imagine that the swift and devastating mortality of the disease made an impact.
Life in a Time of Sudden Death
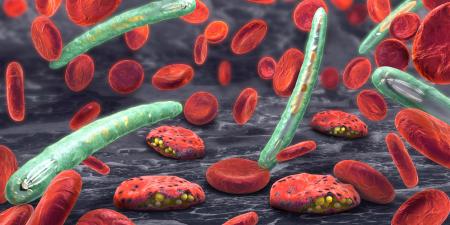
The first wave of the Black Death occurred between 1347 and 1351, arriving most likely from China, and killing approximately one quarter to one third of the European population within 2 years [3]. In some locations, historians estimate that as much as 60 percent of the population died. After this first onslaught, the plague remained endemic for the next 300 years, returning every so often to cull the population. While epidemics such as the Black Death were dramatic in their devastation, medieval life was accompanied by the constant fear of death. Even without the plague, the average life expectancy for women was about 29 years and for men, only 28. In such harsh times, the greatest fear of all was mors improvisa, an unexpected death coming before confession and forgiveness of sin [4]. This fear only increased during the plague when hundreds of thousands of people sickened and died, often within just a few days. It was also this fear which “gave rise to a genre of devotional literature designed to inspire good works and foster an appropriate sense of contrition in the reader” [5].
Henry’s text is one example of confessional works designed to invoke contrition. The first half of the Book of Holy Medicine is devoted to descriptions of his sins as wounds that afflict various parts of his body—the head, eyes, ears, nose, mouth, hands, and heart. Henry portrays himself as the patient and Christ as the physician. In one passage, he describes his sin as an open wound that needs treatment, saying,
“I could have helped myself and cut off the [festering] limb by true confession and repentance of the heart…I should have chastened my flesh and cut away, not only the fire of sin, but the heat of the flesh by abstinence and other hardships, so that the fire’s passage would have been cut off, so that it could have gone no further” [6].
In addition to spiritual healing, as a nobleman Henry of Lancaster would have had access to the best medical care, even though it would have been of little help in the face of the plague. In addition, the accidents, injuries, and diseases responsible for the short life spans of the time were largely beyond the scope of the medieval medical practitioner to cure. As a result, medieval physicians focused largely on prevention.
Medicine during the Middle Ages was conducted by a wide variety of practitioners, ranging from herbalists and conjurers to surgeons and university-trained physicians. Though there were some differences between medical training in Oxford and in Europe, they were largely similar with emphasis placed on theology and liberal arts for the first 7 years, followed by 3 additional years of study to obtain an “MD degree” [7]. Liberal arts training included the trivium(grammar, logic, and rhetoric) and the quadrivium (mathematics, music, geometry, and astronomy). As reflected in the trivium, reasoning, discussion, and debate were the skills most important to be learned. Further medical training was largely provided by set texts, mainly classic medical authors including Avicenna and Galen [7]. Some universities required clinical training with a physician (to be arranged by the student) and still others, particularly in Bologna and Montpelier in the early to mid-1300s, required attendance at an anatomical dissection. But the basis of becoming a physician rested on one’s ability to know the reasons for sickness and to know how illness fit into an intellectual theory about health. It was this intellectualism that was critical to distinguishing “the learned physician who knew the reasons for things [from] the hireling with a knack for healing” [7]. Many physicians had taken holy orders of some kind [8].
Surgery was a distinctly separate and, for the most part, lesser craft and was not widely practiced by physicians, owing in part to the manual labor necessary to perform it as well as to the blood loss inherent to the process. In fact, papal bull forbade clergymen from shedding blood for any reason, including surgical procedures. Following ancient Greek medical theories, university-educated physicians subscribed to the humoral theory of illness and strove to treat disease first by placing it within the appropriate intellectual framework and then by balancing the humors—phlegm (phlegmatic), black bile (melancholic), yellow bile (choleric), and blood (sanguine)—often through purgatives and enemas [4,5].
When Henry of Lancaster began writing his treatise, little was known about how the plague was spread. Multiple theories of its cause were held, from God’s vengeance to contagion to the established medical view that an individual’s susceptibility to plague stemmed from personal imbalance of humors [9]. Physicians stepped into the breach to provide support, medical advice and even spiritual counsel for those wealthy patients who could afford a full-time physician [4]. But, were physicians obligated by any overarching principles of professional ethics to treat the sick during this time of epidemic? Do today’s discussions of personal autonomy or public health ethics have any precedent in the deadly epidemics of the past?
The Medieval Profession of Medicine
In an attempt to discover ethical codes throughout history, some ethicists have proposed at least 3 conditions necessary for the development of a duty-to-treat ethic [1]. First, physicians would have had to recognize that they were at risk of becoming infected. Theories of contagion and polluted air as causative of disease were present in medieval times and gave rise to the prescription of strong smelling herbs and fumigation with pungent woods as ways to ward off plague [3]. However, the theory of infection and the identification of microorganisms would come many years later. Lacking effective treatments, physicians recommended personal hygiene (such as it was) and well-being as the cornerstones of prevention, with an emphasis on dietary prescriptions to balance the humors.
Second, establishment of a professional ethical code for epidemics requires an organized profession of medicine. With its multiple unlicensed practitioners, the practice of medicine during the mid-14th century was far from organized. The cohesive medical profession we know today simply did not exist in the Middle Ages—“Brewers who practiced surgery, abbots who delivered babies, friars who wrote medical books, a chancellor of the exchequer who doctored the king, a Cisterician surgeon—all were involved in healing, and all were involved in other pursuits” [10].
While the Hippocratic Oath was certainly known to medieval physicians, there is little evidence that it substantially influenced their practice [11]. The ethical principles of beneficence and nonmaleficence have been found in Hippocratic writings, although the actual precept of primum non nocerecannot be directly attributed to Hippocrates despite many attempts to do so [12]. Furthermore, the Hippocratic Oath did not set forth ethical principles for the event of an epidemic but focused instead on the patient-physician relationship. And even these principles were not universally acknowledged; during the medieval plague years, the prevailing wisdom was simple: “flee early, flee far, and return late” [13]. It has been noted that something of a duty-to-treat ethic did exist during this time, but it stemmed from the powerful Christian virtues of charity and service to the poor rather than from a sense of professional obligation [1]. These sentiments are certainly echoed in Henry’s Book of Holy Medicine as he consistently appeals to Christ the physician to heal him. “To you, [most sweet Lord] Jesus Christ, I come as to a doctor” [14].
Finally, a public expectation of the duty to treat is necessary for the ideal to take hold; there must be a “social contract” between physician and patient (or even physician and society) that such a duty to treat exists [1]. There is little evidence that such a social contract existed during the Middle Ages. What little expectation there may have been would have likely centered around the notion of the Christian duty to treat the sick.
The history of the medieval plague years throws into stark relief the ethical vacuum that doctors of the time had to fill on their own, falling back on religious convictions, personal compassion, or pragmatic concerns for self-preservation as the basis for their actions. Public expectations of physicians during epidemics are, even today, a point of some contention, with few explicit guidelines on a physician’s duties during an epidemic. Indeed, much of our current discussion of the ethics of epidemics arises from the uncertainty surrounding the responsibilities of either a single physician or physicians as a group during the time of an outbreak. Still, much in the history of medicine and in the social development of the physician remains unknown. In the face of limited evidence, we must remember,
Perhaps the most celebrated physician ever is Hippocrates yet we know literally nothing about him. Neither do we know anything concrete about most of the medical encounters there have ever been. The historical record is like the night sky; we see a few stars and group them into mythic constellations. But what is chiefly visible is the darkness [4].
References
- Huber SJ, Wynia MK. When pestilence prevails: physician responsibilities in epidemics. Am J Bioeth. 2004;4(1):W5-W11.
-
Henry’s text is written in Anglo-Norman. For this paper, quotations are taken from EJ Arnould’s edition of the manuscript published by the Anglo-Norman Text Society. Henry of Lancaster. Le Livre de Seyntz Medicines (The Book of Holy Medicine). Arnould, EJ, ed. Oxford, UK: Anglo-Norman Text Society; 1940. No complete modern English translation of Henry’s work exists, but an excerpt has been translated into modern English in Bartlett AC, Bestul TH. Cultures of Piety: Medieval English Devotional Literature in Translation. Ithaca, NY: Cornell University Press; 1999:19-40.
-
Porter R. The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present. London, UK: Fontana Press; 1997:122
-
Rawcliffe C. Medicine and Society in Later Medieval England. London, UK: Sandpiper Books Ltd; 1995. 1-28, 105-125.
-
Rawcliffe C, 5. See also Hanley M. Medieval Themes and Topics.Available at: http://www.wsu.edu/~hanly/chaucer/coursematerials/humours.html. Accessed March 27, 2006.
-
Henry of Lancaster, 165, lines 16-18, 21-27. Author's translation.
-
Porter R, 114.
-
Porter R, 110.
-
Porter R, 124-125.
-
Getz F. Medicine in the English Middle Ages. Princeton, NJ: Princeton University Press; 1998:19.
- Davey LM. The oath of Hippocrates: an historical review. Neurosurgery. 2001;49(3):554-566.
-
Smith CM. Origin and uses of primum non nocere—above all, do no harm! J Clin Pharmacol. 2005;45(4):371-377.
-
Porter R, 123.
-
Henry of Lancaster, 159, lines 1-5. Author's translation.