Abstract
Background: There is a lack of African American (AA) community engagement in genomic medicine research. Recent popular interest in the experience of AAs, such as that of Henrietta Lacks, has perhaps prompted interest in research on how AA nurses can provide strategies to better engage AA communities in genomic medicine research.
Methods: The authors conducted one-on-one semi-structured interviews with 11 National Black Nurses Association (NBNA) chapter leaders from 8 different US states, representing 782 NBNA members.
Results: Our results quantified NBNA chapter leader agreement on known themes from the literature, captured newly emerging themes, and produced a set of actionable strategies to help overcome barriers to AA engagement in genomic medicine research that fall under 6 themes: (1) engagement, support, information dissemination, and implementation recommendations in general and to address health disparities; (2) addressing language barriers; (3) addressing research implementation barriers; (4) getting physicians to participate; (5) overcoming privacy concerns; and (6) nursing education recommendations.
Conclusions: Actionable strategies presented herein can help researchers better engage AA communities in genomic medicine research.
Introduction
There is a lack of ethnic diversity in clinical research, especially genomic medicine research, which affects understandings of gene-disease relationships. About 78% of data used in genome-wide associational studies (GWAS) comes from people of European descent, but this particular group makes up only 16% of the global population.1 What has resulted is European bias in risk prediction of genetic diseases and other genomic applications in medicine in populations of non-European descent.1 However, European bias in studies like GWAS can be addressed through greater inclusion of more global populations of non-European descent, such as diverse African American (AA) populations.
Nurses have a role to play in furthering this goal as caregivers who often serve as liaisons or bridges between physicians and patients and as health educators in medical, research, and diverse community settings (eg, community clinics, schools, places of worship). They often serve as educators on key clinical topics that include but are not limited to health care quality, efficiency, and safety; the provisioning of health care services; population health management; and informed consent in clinical research and genomic medicine research.2,3,4,5 Thus, AA nurses are well placed as partners for promoting the importance of racial/ethnic diversity in genomic medicine research.
Indeed, the National Black Nurses Association (NBNA) recognized the opportunity for AA nurses to contribute to increasing the ethnic diversity of genomic medicine research, as such research could clinically benefit AAs and other populations of color. NBNA chapters have recently shared with their members the importance and goals of the National Institute of Health’s (NIH) All of Us Research Program,6 a national and inclusive genomic medicine research program with a stated goal to extend genomic medicine to all diseases by building a national research cohort of 1 million or more US participants.7 Ethical issues and concerns, such as confidentiality and trust, based on historical clinical research that involved AAs were also key topics of discussion.6 These concerns resonated with those expressed by AA nursing professionals and members of the health science community during a recent public event.6,8
There is great opportunity to engage AA nurses as partners in genomic medicine research promotion. Results from All of Us Research Program postengagement evaluation surveys,6 along with a paucity of qualitative evidence on AA nurses’ perspectives on and concerns about this topic, have unveiled a need to explore appropriate ways to increase AA participation in genomic medicine research. Building on our literature review,8 we sought to elucidate AA nursing professionals’ views on this topic but, more importantly, to identify possible strategies to overcome any concerns they or AA patients might have based on their perspectives.
Methods
We conducted in-depth one-on-one interviews with NBNA chapter leaders only (to operate within our pilot project budget and timeline) who have experience, knowledge, or awareness of precision or genomic medicine research. Through closed- and open-ended questions, we sought to (1) identify AA nurse leaders’ perspectives on and experiences with what might influence their own and AA patient/community participation in genomic medicine research and (2) explore and identify, based on those nurses’ views, strategies to overcome or address those concerns. Interviews allowed us to further build a dialogue with the NBNA chapter leaders, giving them dedicated time and space to highlight arguments and experiences that they personally, and on behalf of their chapters, felt were pertinent and worthy of discussion or consideration. This study followed the Standards for Reporting Qualitative Research reporting guideline.9
Sample. According to the NBNA chapter directory, in 2019, when the project began, there were 9667 members across 118 NBNA chapters in 33 states, with an average of 82 members and a range of 23 to 141 members per chapter. A chi-square test for homogeneity showed no significant relationship between the number of members per NBNA chapter and the state in which chapters are located (P > 0.05). Therefore, all NBNA chapter leaders, regardless of chapter location, were openly invited to participate in interviews, and all volunteers were interviewed. Interviews were conducted with 11 NBNA chapter leaders in 8 different US states (Ohio, Illinois, Alabama, California, Michigan, Louisiana, New York, Arizona), representing 782 NBNA chapter members. Many of the chapter members were familiar with precision or genomic medicine research either through direct involvement in research (personal or professional) or through witnessing involvement of close colleagues or relatives.
Interview guide. Our prior work enabled us to identify several concerns that NBNA members had about AA patient/community engagement in genomic medicine research through a literature review 6,8 that led to the development of our interview guide. Closed-ended interview questions allowed us to determine if the NBNA chapter leaders agreed or disagreed with concerns identified in our prior work,8 and open-ended questions allowed us to identify new, emerging themes and strategies to overcome those concerns. The interview guide was piloted among the research team members and South Nevada Black Nurses Association (SNBNA) chapter members and colleagues with experience in qualitative research. (Pilot interviews were excluded from the final data set.)
Interviews and transcription. Interviews were conducted by telephone in the English language from December 2019 to March 2020 by the second author (L.M.E.) and recorded with participants’ consent. Prior to interviews, interviewees received a brief explanation of the study’s purpose and scheduled a convenient time for the interview. Oral informed consent was obtained from all interviewees at the start of the interview. L.M.E. explained to each interviewee how their personal identifiable information would be kept confidential and anonymous. Interviewees were informed that they could skip or refuse to answer any question if they wished and could stop the recording at any time.
The duration of all interviews ranged between 22 and 59 minutes (median duration of 31 minutes). The observed range in interview time duration was largely due to the fact that some interviewees had more insights or experiences to contribute or draw upon during the interviews than others. We calculated the percentage agreement with themes identified in our previous work related to member concerns,8 and new themes encapsulating members’ further concerns were identified. Strategies to overcome concerns related to these themes were identified and encapsulated in actionable themes. Interviews were transcribed verbatim by a third-party transcription service provider, and transcripts were checked for accuracy and clarity against the audio recordings.
Data analysis. The first author (R.M.H-S.) analyzed interview data using NVivo software and carried out inductive data coding (to quantify agreement with known themes and number of quotations falling into new theme categories) and deductive data coding (to identify and develop new categorical and actionable themes) in Microsoft Excel, using constant comparative analysis in accordance with the grounded theory approach.10 The third author (T.J-G.) served as a second coder to assess percentage agreement among coders and interrater reliability. The resulting codes were built into categorical and actionable themes that were deliberated upon and discussed among members of the research team until strong (> 95%) agreement was reached.
Results
Interviewee agreement on known themes. Table 1 presents interviewee agreement with concerns identified in our literature review8 that might influence their own or AA patients’/communities’ participation in research. The majority (90%) of NBNA member interviewees agreed that these concerns pose barriers to participation in research.8 The strongest (100%) agreement among NBNA member interviewees was found for 3 concerns: (1) genomic health information privacy, (2) how precision medicine can be leveraged to address existing—or to prevent exacerbating—health disparities, and (3) insufficient physician willingness to engage in precision medicine research.
|
Concerns Posing Barriers to Research Participation |
% Agreement |
|---|---|
|
Health information privacy |
100 |
|
Precision medicine addressing health disparities |
100 |
|
Physician willingness to participate in or conduct precision medicine research |
100 |
|
Understanding target audiences among AA communities for promoting precision medicine research |
91 |
|
Costs to participation in precision medicine research |
82 |
|
Language barriers |
64 |
|
Average/overall agreement |
90 |
The least agreement (64%) was found for language barriers. Interviewees who disagreed that language poses a barrier to research participation felt that, within their local communities, AA residents largely spoke the same language (English). However, interviewees in disagreement emphasized the importance of avoiding jargon. As one put it, “I think if we wanted to do better instead of maybe looking at different languages, maybe looking at people who can explain it in a way or essentially convert the information in our medical terminology, in our health care jargon to a way that they understand it.”
A large majority (91%) of interviewees agreed that insufficient understanding of who the target audience should be when promoting precision medicine research is a barrier to AA patient/community participation in genomic medicine research because effective health promotion and engagement within AA communities often occurs outside of traditional patient settings.11,12,13 The interviewee who disagreed with this concern had had successes in reaching nursing and other medical professionals, also a target audience: “We haven’t explored it specifically that way, I think, because we, our focus was really reaching out to nurses and medical professionals...”
A majority (82%) of interviewees also agreed that costs of participation in precision medicine research is a barrier. However, 2 interviewees disagreed because they viewed patients’ personal costs of participation (eg, childcare for clinic visits, transportation costs) as an understandable but not a major concern in practice and noted that participants receive compensation for research participation. One interviewee stated: “the vast majority of people that we would need to participate in research are patients who would be getting reimbursed… and are not coming from private insurances. That’s paid up front.”
Emergent themes. Seven themes emerged from analysis of the interviews reflecting additional concerns of AA nurse interviewees (see Table 2 and Figure). These themes are (1) authenticity in outreach, (2) patient empowerment/activation, (3) research retention, (4) accountability for responsible conduct of research, (5) informed consent, (6) physical location/proximity to research centers, and (7) communication with general health care professionals about research participation.
|
Newly Emerging Theme |
Theme Description |
|---|---|
|
Authenticity in outreach |
Making sure that community outreach is done by individuals who understand, share, and appreciate the culture of the community. |
|
Patient empowerment/activation |
Ensuring that patients feel personally empowered and engaged as partners in the management of their own health rather than used or undervalued. |
|
Research retention |
Encouraging and inspiring individuals to stay engaged in the research process following initial enrollment. |
|
Accountability for responsible research conduct |
Ensuring that researchers adhere to standards of research ethics and rigor and are held accountable for how they design, conduct, and report research findings or data about AAs. |
|
Informed consent |
Ensuring comprehension of and full transparency about all aspects of the research, including data management and sharing, biospecimen storage and retention, and outcomes being assessed. |
|
Physical location/proximity to research centers |
Concern that residents of rural communities must find transportation to participating research centers, often located in cities. |
|
Communication with routine health care professionals about research participation |
Involving individuals’ primary care or other trusted clinician to keep them aware and informed about their patient-participants’ involvement in precision medicine research. |
Figure. Percentage of Quotations Coded to Each Emergent Theme Based on Interviews
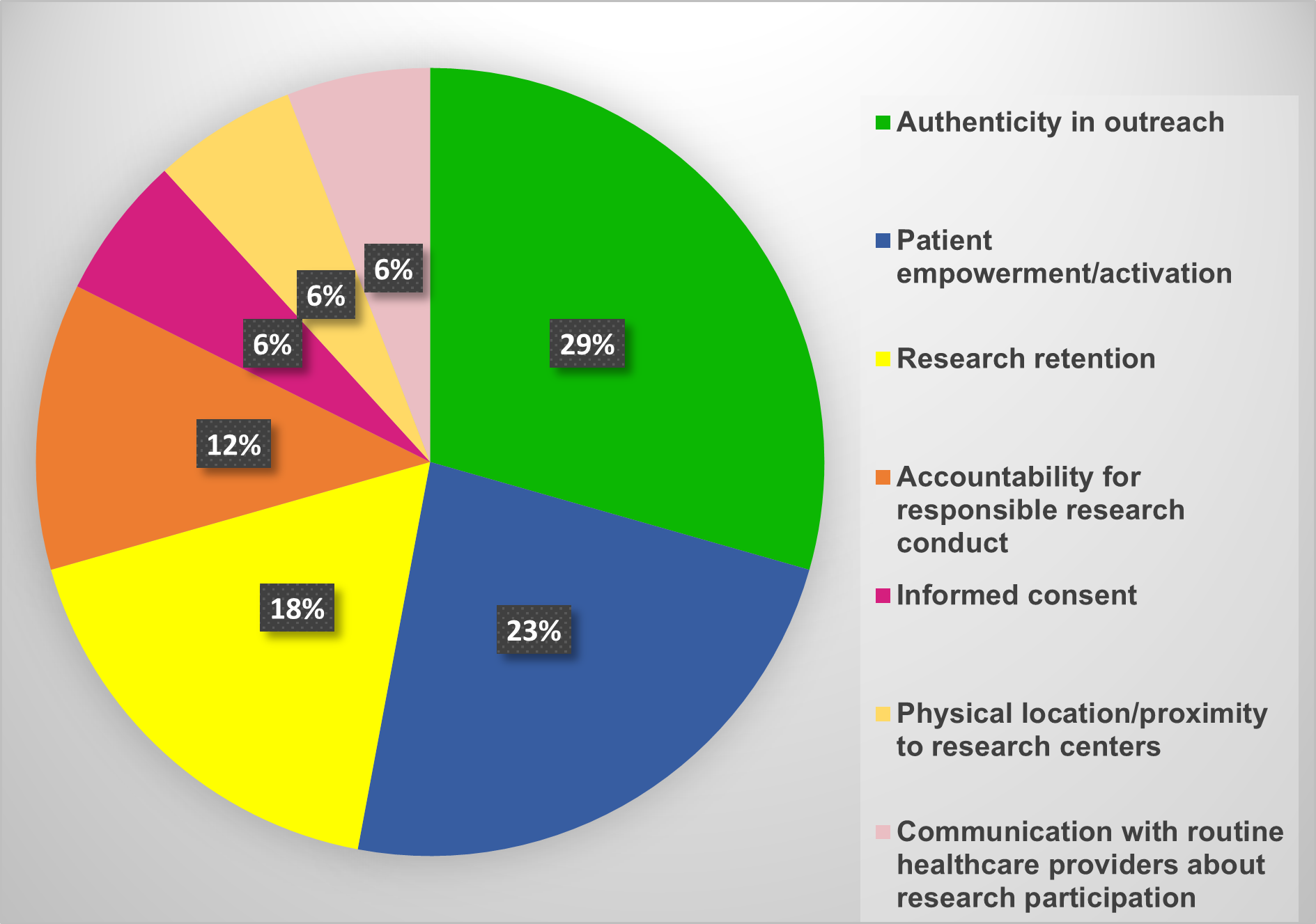
The most frequently expressed theme was authenticity in outreach. Concerns expressed relevant to this theme focused on the historical lack of authenticity in research involving AAs. One interviewee noted: “A lot of participants or people in the community had questions about, okay, how authentic is this? This sounds a lot like the Tuskegee experiment, the Henrietta Lacks issue that was going on.”
Comments under this theme also focused on authenticity in the form of racial/ethnic solidarity. As one interviewee stated: “We’re geared towards Black communities. It could not be non-Black people doing all of the research on the people that we get to sign up…” Another remarked: “And one of the ways that we can push ourselves further up to create equity is by participating in research amongst us, that’s ran by us, that’s then the results presented to us and things of that sort.”
The second most frequent theme was patient empowerment/activation. Concerns related to this theme focused on patient compliance and health beliefs. One interviewee stated: “We have to break that cycle of health care disparity by looking at what it is that we need to do to ourselves to prevent it or to treat it and manage it.” Another commented: “I think one of the bigger things, how we have to combat it, we do need to participate. We’ve come to the realization that we absolutely need to participate in research that is very specific to people who look like us, live like us, live where we live, right?”
The third most frequent theme was research retention, which focused on concerns with continuously engaging with research participants after they have signed up to participate. The size of the problem was recognized by one interviewee: “I think it’s a big issue in terms of how we find new ways of retaining people in the program, particularly, I mean, if we’re talking about a longitudinal study that is going to last a long time.” Similarly, another interview remarked: “I think that’s one of the biggest things that people are saying, okay, you’ve convinced me to sign up. I’ve signed up. Now what?”
Response strategies. All interviewees were asked to contribute their views on possible strategies to overcome their expressed concerns. Interviewees contributed a wide range of actionable strategies that fell under 6 themes: (1) engagement, support, information dissemination, and implementation recommendations in general and to address health disparities; (2) addressing language barriers; (3) addressing research implementation barriers; (4) getting physicians to participate; (5) overcoming privacy concerns; and (6) nursing education recommendations.
Table 3 lists actionable strategies for each of these themes ordered by number of quotations related to each theme.
|
|
|
|---|---|
|
Theme 1: Engagement, Support, Dissemination, and Implementation Recommendations in General and to Address Health Disparities |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Meet communities and individuals where they are. |
30.3 |
|
2. Design and provide specific communication/education tools and strategies (eg, storytelling, focusing on the disease vs the hype of precision medicine). |
24.2 |
|
3. Engage/discuss independent public figures/influencers as partners in and advocates for precision medicine research. |
9.1 |
|
4. Define/describe precision medicine research in a digestible way. |
9.1 |
|
5. Provide an engaged, knowledgeable, and available point-person for participant support (eg, someone who enrolled in and completed the research already, health care professional). |
7.6 |
|
6. Demonstrate immediate and short-term (vs only long-term) benefits and personal benefits to participation. |
7.6 |
|
7. Create a safe setting for dialogue and engagement. |
4.5 |
|
8. Engage family member influencers. |
3.0 |
|
9. Discuss historical research misconduct/mistakes before (not after) engagement. |
3.0 |
|
10. Put research evidence into practice. |
1.5 |
|
Theme 2: Addressing Language Barriers |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Use language that is preferred/understood best by the research participant. |
27.8 |
|
2. Use language interpreters. |
22.2 |
|
3. Use native knowledge or geographic region as an indicator of local language. |
16.7 |
|
4. Be culturally competent to foster trust. |
11.1 |
|
5. Provide translations that are granular enough to account for diversity within African American communities. |
5.6 |
|
6. Account for differences in language translation. |
5.6 |
|
7. Emphasize the importance of tone and nonverbal communication. |
5.6 |
|
8. Tie success in overcoming language barriers to participant follow-through and outcomes. |
5.6 |
|
Theme 3: Addressing Research Implementation Barriers |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Provide extra services, incentives, or reimbursement to absorb participation costs. |
33.3 |
|
2. Inspire authenticity and emphasize benefits of initial and long-term participation. |
25.0 |
|
3. Deploy resources to provide remote access to participation. |
16.7 |
|
4. Conduct lessons learned about research participation. |
8.3 |
|
5. Normalize research and research participation. |
8.3 |
|
6. Overcome perceptions of research “elitism.” |
4.2 |
|
7. Involve primary/usual care clinicians. |
4.2 |
|
Theme 4: Getting physicians to participate |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Focus on the goal of providing high-quality, efficient, patient-centered care. |
33.3 |
|
2. Identify and address reasons for/concerns about physician resistance to participation. |
22.2 |
|
3. Provide/fund abbreviated time and space (remote or in-person) to convene and answer questions. |
16.7 |
|
4. Address/balance conflicting obligations. |
16.7 |
|
5. Foster a culture of educational collaboration between nursing professionals and physicians. |
11.1 |
|
Theme 5: Overcoming privacy concerns |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Be specific about how and why sensitive health information is collected/used. |
22.2 |
|
2. Involve nurses and patients early in the privacy policy-making process. |
11.1 |
|
3. Involve subject matter experts as educators on privacy and data deidentification and security. |
11.1 |
|
4. Address broader gaps in privacy regulation/protection regarding third-party access to sensitive health data. |
11.1 |
|
5. Be transparent about data access/sharing. |
11.1 |
|
6. Emphasize the strengths of existing protection measures. |
11.1 |
|
7. Uphold/monitor research integrity and objectivity. |
11.1 |
|
8. Draw on pivotal successes that resulted from data sharing. |
11.1 |
|
Theme 6: Nursing Education Recommendations |
|
|
Actionable Strategy |
% of All Quotes |
|
1. Include educational curricula on precision medicine and race. |
23.1 |
|
2. Drive home the point and purpose of knowledge dissemination. |
23.1 |
|
3. Distinguish between the reality and hype of precision medicine. |
15.4 |
|
4. Have nurses meet participants where they are and in real time. |
15.4 |
|
5. Make education on precision medicine part of CEUs, foundational courses, and licensing curricula. |
15.4 |
|
6. Include education on advancing technology and health. |
7.7 |
Discussion
New understandings and grassroot insights from our work can empower genomic researchers and research teams—which include nursing professionals—with actionable knowledge. This knowledge is critical to achieve diversity in clinical research, navigate long-held cultural sensitivities within the AA population about engagement in clinical research, and ensure safety and efficacy of treatments guided by genetic testing (eg, pharmacogenomics). AA involvement and participation in genomic medicine research is necessary to further explore the role of genetics and disease, as many studies have used AAs to represent African populations that have greater levels of genetic diversity than non-African populations. Due to AA’s proximal African ancestry, AA gene pools are more diverse than those of populations without proximal African ancestry, as AAs are reported to have the highest percentage (64%) of rare single nucleotide polymorphisms (SNPs) and the lowest percentage of common SNPs (36%).14
Many of the concerns identified in both our literature review8 and qualitative interviews overlap with concerns identified by racial/ethnic minorities in other studies.15,16,17 Thus, the actionable strategies presented herein can indeed be used to improve racial/ethnic minority participation in genomic medicine research. Moreover, our actionable strategies draw on and augment many lessons learned by other researchers seeking to better engage AA communities generally in clinical research. However, more research is needed to determine how these strategies can be applied to engage AA subpopulations with differing cultures, medical conditions, beliefs, and preferences.18
NIH All of Us Research Program investigators reported that, as of July 2019, underrepresented populations compose more than 80% of persons from whom biospecimens have been obtained for research, exceeding their program target of 45%.19 However, the percentage of biospecimens obtained from AA populations was not explicitly stated in this report.19 It is well known that AA communities are uncomfortable with the donation of biospecimens, particularly following revelation of the historical misuse of biospecimens from Henrietta Lacks.20 The All of Us Research Program’s success in recruiting individuals from underrepresented populations is a marker of engagement. However, our findings indicate that there remains a demand to present diverse AA communities with relevant and indispensable information on genomic medicine research and practice; AA communities are most likely to embrace engagement strategies that are based on evidence and also customized for AA communities.
Moreover, the church is a strong influencer in AA communities and can, therefore, inspire movement and change on many topics that are important to AAs, such as health and family wellness.21 Thus, it would be prudent to seek churches’ buy-in and engage AA clinicians that attend church to inspire participation. AA nurses, doctors, and pastors—as well as the professional or community organizations they represent, such as the NBNA—all have influence in AA communities and thus have opportunities to implement and to evaluate the effectiveness of the actionable strategies within and across local contexts and practice or outreach settings. For example, the NBNA’s previous participation in All of Us Research Program engagement initiatives6 provides opportunity for NBNA members’ continued engagement through the implementation of the actionable strategies in medical, community, or research practice settings with patients or research participants and other clinicians.
A key limitation of our study is the relatively small number of interviewees (11 total) and low US state representation (only 8 out of 50 US states). The interviewees were chapter leaders who directly and positively responded to our broad and open interview invitations, which stated up front our intent to discuss and describe NBNA chapter members’ thoughts and concerns about genomic medicine research. To enhance the richness of our data, we purposively interviewed NBNA chapter leaders (eg, chapter board members) who felt that their views reflected those of their chapter, particularly given the feedback or responses they received during prior NBNA engagement initiatives with the All of Us Research Program.6 However, no additional attempts were made to assess interviewees’ claims that their views represented those of their chapter members. Nevertheless, we believe we have begun the process of capturing and amplifying the voices of AA nurse community leaders’ lived experiences and insightful perspectives.
Conclusion
AA nurses, as influential stakeholders within AA and other communities, are instrumental to promoting engagement in genomic medicine research. This study presents actionable strategies to help overcome AA communities’ long-held concerns and beliefs about clinical research and mistrust of clinical researchers, which is a necessary next step to help improve the racial/ethnic diversity of research participants.
References
- Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet. 2019;51(4):584-591.
- Rhodes D, Visker JD, Cox C, Sas A, Banez JC. Effects of an online educational module on school nurses’ knowledge of HPV vaccination. J Contin Educ Nurs. 2017;48(9):431-436.
- Bleich MR. The professional development educator role in leading population health management. J Contin Educ Nurs. 2018;49(11):496-497.
- McKown T, McKeon L, Webb S. Using quality and safety education for nurses to guide clinical teaching on a new dedicated education unit. J Nurs Educ. 2011;50(12):706-710.
- Stalter AM, Mota A. Recommendations for promoting quality and safety in health care systems. J Contin Educ Nurs. 2017;48(7):295-297.
-
National Black Nurses Association. NBNA News (theme issue, “All of Us” Research Program). 2019. Accessed October 12, 2020. https://www.nbna.org/files/all%20of%20us%20special%20issue%20NBNA%20news.pdf
-
All of Us Research Program overview. National Institutes of Health. Accessed October 12, 2020. https://allofus.nih.gov/about/about-all-us-research-program
-
Hendricks-Sturrup RM, Edgar LM, Johnson-Glover T, Lu CY. Exploring AA community perspectives about genomic medicine research: a literature review. SAGE Open Med. 2020;8:2050312120901740.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245-1251.
-
Chun Tie Y, Birks M, Francis K. Grounded theory research: a design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927.
-
Holt CL, Shelton RC, Allen JD, et al. Development of tailored feedback reports on organizational capacity for health promotion in African American churches. Eval Program Plann. 2018;70:99-106.
-
Santos SL, Tagai EK, Scheirer MA, et al. Adoption, reach, and implementation of a cancer education intervention in African American churches. Implement Sci. 2017;12(1):36.
- Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med. 2018;378(14):1291-1301.
- Campbell MC, Tishkoff SA. African genetic diversity: implications for human demographic history, modern human origins, and complex disease mapping. Annu Rev Genomics Hum Gene. 2008;9(1):403-433.
- George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16-e31.
-
Fisher ER, Pratt R, Esch R, et al. The role of race and ethnicity in views toward and participation in genetic studies and precision medicine research in the United States: a systematic review of qualitative and quantitative studies. Mol Genet Genomic Med. 2020;8(2):e1099.
- Clark LT, Watkins L, Piña IL, et al. Increasing diversity in clinical trials: overcoming critical barriers. Curr Probl Cardiol. 2019;44(5):148-172.
- Hussain SB, Quittner AL, Brown M, Li-Rosi AM. Understanding access to genomics in an ethnically diverse South Florida population: a comparison of demographics in Odyssey and rapid whole genome sequencing programs. J Genet Couns. 2020;29(4):553-561.
-
Denny JC, Rutter JL, Goldstein DB, et al; All of Us Research Program Investigators. The “All of Us” Research Program. N Engl J Med. 2019;381(7):668-676.
- Lee SS, Cho MK, Kraft SA, et al. “I don’t want to be Henrietta Lacks”: diverse patient perspectives on donating biospecimens for precision medicine research. Genet Med. 2019;21(1):107-113.
-
McNeill LH, Reitzel LR, Escoto KH, et al. Engaging Black churches to address cancer health disparities: Project CHURCH. Front Public Health. 2018;6:191.



