Abstract
The Indian Health Service (IHS) administers health care services to American Indians and Alaska Natives (AI/ANs) in the United States. The agency funds referral care services through the Purchased/Referred Care (PRC) Program, which prioritizes its budget to pay for emergent care. This commentary responds to a case about a physician’s disappointment that a referral for nonemergent care is deferred for payment by the PRC Program. Jonsen et al’s 4-quadrant approach (a microethical case analysis model) is applied to suggest that deferring referrals is just only when the PRC Program operates fairly. This model, however, might inadequately account for structural inequities underlying referral care rationing by the IHS, a federal entity that is legally and ethically obligated to care comprehensively for AI/AN patients.
Case
At an Indian Health Service (IHS) facility in Wyoming, a state in which Medicaid coverage has not been expanded under the Affordable Care Act, pediatric and gynecologic care is available inconsistently, and surgical and other subspecialty care is not offered. Dr R previously worked in the academic sector and was recently hired as a primary care physician at this IHS site. On his first day, he joins administrators and clinicians who meet regularly in the Purchased/Referred Care (PRC) Review Committee to review referral requests for health care services unavailable at the facility. In IHS sites without specialists, government funding can be directed to non-IHS public or private health care organizations to purchase needed specialty care for AI/AN patients. However, referral requests for nonemergent services are rarely approved at Dr R’s and other IHS sites due to insufficient federal funding.
During the meeting, a referral for Ms B is discussed. Ms B is a 55-year-old patient with bilateral knee osteoarthritis and disabling knee pain, and her IHS clinician placed a referral for an orthopedics consultation to assess her candidacy for surgical intervention. Ms B gets around with a wheelchair and manages her pain with opioids. She does not have private or public insurance. Dr R and his clinical colleagues agree that the referral is medically indicated, but authorization for payment of Ms B’s referral is deferred by the committee because her medical need is deemed chronic and not emergent.
Dr R is distressed about the PRC Review Committee’s decision and the limited medical services that can be offered to Ms B, particularly when compared to resources accessible to publicly and privately insured patients with similar health care needs at his previous clinic.
Commentary
The IHS is a federal agency within the US Department of Health and Human Services that administers health care services to approximately 2.6 million American Indians and Alaska Natives (AI/ANs),1 who have legal rights to medical care per the trust obligation of the US government to tribal nations.2 Unlike Medicare and Medicaid, the IHS is neither an entitlement program nor an insurance program. The agency is primarily financed through discretionary congressional appropriations and revenue from third-party collections (eg, Medicare, Medicaid, Veterans Administration, Children’s Health Insurance Program, private insurers).1 A portion of the IHS budget is used to authorize referral care, defined as health care services unavailable in IHS facilities, through the PRC Program.3 Specific regulations exist for “stretch[ing] the limited PRC dollars,” thus permitting referral care via agency-wide rationing.4
As an enrolled member of a federally recognized tribe, Ms B qualifies for medical services offered directly at the IHS facility. Ms B has obtained primary care services and is referred for orthopedics care unavailable at her IHS site. A referral placed by an IHS clinician like Dr R does not guarantee its authorization for payment by the PRC Program; authorization requires that the referral meet criteria defined by the Code of Federal Regulations and the Indian Health Manual.5
IHS PRC Program Criteria
Residency requirement for the PRC Program. For Ms B’s orthopedics referral to be authorized by the PRC Program, her permanent residence must be within a PRC delivery area (PRCDA). This requirement ensures that limited PRC funds are allocated to patients living in counties on or near tribal lands. If Ms B does not reside within her IHS site’s PRCDA or meet criteria for special cases, her referral will be denied for payment by the PRC Program.6
Requirement for notifying the PRC Program. Except in the case of an emergency, a referral must be reviewed by the PRC Program before any associated referral care services are accessed.7 If this notification requirement is not met, Ms B’s referral will be denied for payment by the PRC Program.
Resource stewardship from a lens of equality alone is inadequate in this case.
Assignment of a medical priority rating by the PRC Review Committee. When funds are insufficient to pay for all referrals submitted to the PRC Program at an IHS facility, referrals are authorized based on “relative medical priority”8,9 using policy-based allocation criteria that prioritize “those most in need.”9 Medical documentation for Ms B’s referral services was reviewed and her referral assigned a priority ranking by her facility’s PRC Review Committee, a group of administrative and clinical staff, according to the following levels: (I) emergent or acutely urgent, (II) preventive, (III) primary and secondary, (IV) chronic tertiary, and (V) excluded.10 Referrals for services deemed by PRC Review Committees to be level I are authorized for payment by the PRC Program at most IHS sites, and those deemed levels II to V are authorized based on available funds, referral volume, and “relative medical need.”11 If Ms B’s referral is not assigned a priority ranking that permits payment authorization by her site’s PRC Program, it will be deferred until funds are available.
Use of alternate resources. PRC Programs do not authorize payment for referrals unless IHS beneficiaries like Ms B utilize other resources (ie, Medicaid, Medicare, and private insurance) for which they are eligible. The IHS is a “payor of last resort”12 and only authorizes payment for referral care services not covered by other payers.12,13
Ms B’s Case in 4 Quadrants
We analyze this case using Jonsen, Siegler, and Winslade’s 4-quadrant model, a framework for clinical ethics case analysis that applies Beauchamp and Childress’ biomedical principles (ie, beneficence, nonmaleficence, autonomy, and justice) to 4 case-specific areas (quadrants): medical indications, patient preferences, quality of life, and contextual features.14,15 To focus our case analysis on contextual features of resource scarcity and rationing, we assume that Ms B is eligible for her IHS facility’s PRC Program, that available funding restricts payment authorization to level I referrals, and that Dr R regards Ms B’s referral as indicated, aligned with current best-practice standards for osteoarthritis management, and in accordance with her preferences and quality of life. Dr R and his PRC Review Committee colleagues must assign a priority ranking for her referral care services.
Orthopedics intervention is standard of care for patients experiencing disabling pain and compromised functioning due to moderate and severe osteoarthritis.16 Ms B is appropriately referred to orthopedics services to address her chronic pain and to improve her mobility. Orthopedics intervention might help reduce prescription opioid use; manage comorbid obesity, endocrinopathies, and cardiovascular diseases, if present; and improve co-existing social determinants of health.17
Dr R and his colleagues in the PRC Review Committee are obligated to assess Ms B’s medical need for orthopedics care relative to medical needs of other PRC-eligible patients at the IHS facility and assign the commensurate priority ranking. We expect Ms B’s referral is deemed level III, and it will be deferred due to insufficient funding to pay for non-level I referrals. Through a 4-quadrant microethical lens, this might be ethically appropriate, provided that the PRC Program fairly and equally reviews referrals for PRC-eligible patients at the site. Macroethical historical, political, and cultural considerations are also relevant in Ms B’s case, however, and they are inadequately integrated into our case analysis if considered only as features of the “context” quadrant rather than the foundation of the quadrant itself.
Four Quadrants Is Not Enough
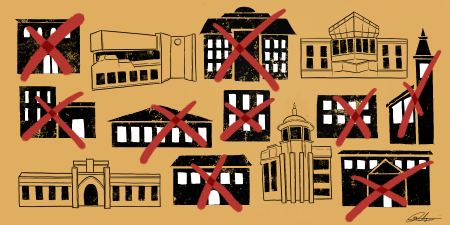
The US government’s trust obligation to tribal nations incorporates legal rights for AI/ANs to health care services.2 This provision deserves fuller consideration than that afforded by the 4-quadrant model, as it is a unique determinant of health equity and justice. The historical and legal circumstances surrounding AI/AN health care in the United States is key to understanding Dr R’s distress about Ms B’s referral outcome.18 Dr R cannot immediately remediate the inequities inherent in disproportionately lower per capita health care expenditures by the IHS relative to public and private health insurers in the United States, nor can he modify the structural framework by which an IHS PRC Program authorizes referral payment for nonemergent care according to (1) a patient’s geographic proximity to an IHS facility, (2) a patient’s eligibility for insurance, and (3) whether and to what extent a patient’s disease state is emergent or end-stage. Dr R, his IHS facility, and the IHS as an agency are ethically obligated to steward scarce resources fairly and equally through the PRC Program (see Table). However, resource stewardship from a lens of equality alone is inadequate in this case. Inequities in AI/AN health are exacerbated by the federal government’s failure to meet its legal obligation “to ensure the highest possible health status for Indians and urban Indians and to provide all resources necessary to effect that policy.”19 When this macrolevel lens is applied, Dr R is likely to see that the PRC Program’s decision about Ms B’s referral is fundamentally unjust.
|
Goal |
Action |
|---|---|
|
Clinician |
|
|
Counsel patients on the PRC Program’s policies and operations at the time of referral submission. |
- Screen for barriers to patient eligibility for the PRC Program as part of routine health care. - Provide anticipatory guidance to patients on the likelihood of a referral’s authorization and appeals processes for denials. |
|
Submit referral requests with concise and thorough documentation of the medical indication(s) without identifying or biasing information. |
- Document clear diagnoses and associated aspects of evaluation and case management that corroborate a referral request and its medical priority level. - Deidentify all patient cases and omit patients’ insurance status in committee discussions. |
|
Ensure the referring clinician is present in committee to discuss patient referrals. |
- Support completeness and accuracy of the committee discussion of a referral. - Contribute to the determination of the referral’s medical priority level. |
|
IHS Facility |
|
|
Ensure consistent and comprehensive membership in committee meetings over time. |
- Provide administrative time for clinicians to attend PRC Review Committee meetings on a routine basis. - Ensure all committee meetings include clinical membership sufficient to adjudicate the medical indication(s) and priority level of referrals. |
|
Promote consistency of funding within and across periods of the fiscal year. |
- Submit referrals to the PRC Program for all medically necessary needs regardless of insurance status, eligibility, and anticipated likelihood of PRC authorization. - Develop facility-wide processes for assessing public insurance eligibility and supporting patient enrollment in these programs. - Hire and maintain case management staff to support care coordination for PRC-eligible patients with referral needs. |
|
Advocate for offering more comprehensive direct care services. |
- Advocate for hiring and retaining specialty-trained clinicians. - Support CME for general medicine clinicians to gain specialty skills. - Provide clinical and administrative time for IHS clinicians to connect with low-barrier, cost-effective specialty programs like Project ECHO.20,21 |
|
Reflect on the barriers and limitations to fair and equal access to PRC funding for IHS-eligible patients. |
- Maintain accurate contact information, including mailing addresses. - Counsel patients on the importance of written notifications for receiving updates on eligibility for PRC funding and appealing PRC denials or deferrals. |
|
IHS Agency |
|
|
Develop local and agency-wide processes to address COIs within the PRC Program. |
- Amend existing PRC Program policy to define personal and professional COIs and associated resolution processes. |
|
Reflect on the tenets of the IHS medical priorities of care, with attention to preventive care. |
- Discuss and frame level I needs in relation to chronic disease management and preventive health. - Define the policy underlying “relative medical need”11 and its application to referrals meeting the same priority level. |
|
|
Recommendations
Unjust referral care rationing within the IHS warrants tribal, state, and federal attention. Health equity is not achievable without such a 3-pronged effort to remediate injustice, promote equity, and advocate for AI/AN patients. The current rationing system assumes it is cost-effective to prioritize emergent care over preventive or chronic disease care, but whether and to what extent evidence supports this assumption requires investigation. Medicaid and Medicare enrollment should be championed for all IHS-eligible patients, as expansion of these programs in states in which tribal nations reside will increase PRC Program capacity to fund more referral care.22 Federal appropriations to the IHS must be adequate to reliably meet AI/AN health care needs and promote equity.23 The determination that the IHS be regarded as a “payor of last resort”12 warrants legal and ethical scrutiny as to whether and how this element of policy undermines the federal government’s trust obligation to tribal nations.2 Finally, tribal nations’ sovereignty must be respected, and tribes must be championed to design and administer health infrastructure that elevates their citizens’ health in ways that produce and sustain equity.
References
-
IHS profile. Indian Health Service. August 2020. Accessed November 18, 2020. https://www.ihs.gov/newsroom/factsheets/ihsprofile/#:~:text=Indian%20Health%20Service%20(IHS)%20direct,and%20tribally%20managed%20service%20units
-
Native American health: historical and legal context: federal trust relationship. In: National Academies of Sciences, Engineering, and Medicine. Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press; 2017:Appendix A.
-
Farb J. Indian Health Service: spending levels and characteristics of IHS and three other federal health care programs. US Government Accountability Office. December 10, 2018. GAO-19-74R. Accessed August 31, 2020. https://www.gao.gov/assets/700/695871.pdf
-
Purchased/referred care (PRC): history. Indian Health Service. Accessed August 31, 2020. https://www.ihs.gov/prc/history/
-
Purchased/referred care (PRC): requirements: eligibility. Indian Health Service. Accessed August 31, 2020. https://www.ihs.gov/prc/eligibility/requirements-eligibility/
-
Purchased/referred care (PRC): requirements: purchased/referred care [PRC] delivery areas. Indian Health Service. Accessed August 31, 2020. https://www.ihs.gov/prc/eligibility/requirements-purchased-referred-care-prc-delivery-areas/
-
Purchased/referred care (PRC): requirements: notification. Indian Health Service. Accessed August 31, 2020. https://www.ihs.gov/prc/eligibility/requirements-notification/
-
Indian Health Service. Indian Health Manual. Part 2: chapter 3—Purchased/referred care. Section 2-3.7: purchased/referred care medical priorities. Accessed August 31, 2020. https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.7
-
Indian Health Service. Understanding the Purchased/Referred Care Program: part 4. Director’s Blog. September 22, 2011. Accessed August 31, 2020. https://www.ihs.gov/newsroom/directorsblog/september2011/
-
Indian Health Service. Indian Health Service medical priority levels. Manual Exhibit 2-3-B. Accessed August 31, 2020. https://www.ihs.gov/sites/ihm/themes/responsive2017/display_objects/documents/pc/58619-1_Manual_Exhibit_2-3-B_IHS_MedicalPrioritiesRolesAndResponsibilities.pdf
-
Indian Health Service. Indian Health Manual. Chapter 3—Purchased/referred care. Section 2-3-20. Accessed August 31, 2020. https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.20
-
Indian Health Service. Indian Health Manual. Part 2: chapter 3—Purchased/referred care. Section 2-3.8: payor of last resort requirements. Accessed August 31, 2020. https://www.ihs.gov/ihm/pc/part-2/chapter-3-purchased-referred-care/#2-3.8
-
US Government Accountability Office. Indian Health Service: facilities reported expanding services following increases in health insurance coverage and collections. September 2019. GAO-19-612. Accessed August 31, 2020. https://www.gao.gov/assets/710/701133.pdf
-
Jonsen AR, Siegler M, Winslade WJ. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. 8th ed. McGraw-Hill; 2015.
-
Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 7th ed. Oxford University Press; 2012.
-
American Academy of Orthopaedic Surgeons. Surgical Management of Osteoarthritis of the Knee: Appropriate Use Criteria. December 9, 2016. Accessed August 31, 2020. https://www.aaos.org/globalassets/quality-and-practice-resources/surgical-management-knee/smoak-auc_hardcopy-treatment_1.4.171.pdf
-
Artiga S, Hinton E. Issue brief: beyond health care: social determinants in promoting health and health equity. Kaiser Family Foundation. May 10, 2018. Accessed August 31, 2020. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
-
National Indian Health Board. The National Tribal Budget Formulation Workgroup’s Recommendations on the Indian Health Service Fiscal Year 2021 Budget. April 2019. Accessed August 31, 2020. https://www.nihb.org/docs/04242019/307871_NIHB%20IHS%20Budget%20Book_WEB.PDF
-
Indian Health Care Improvement Act, 25 USC §1602 (2020).
-
Indian Country ECHO website. Accessed September 1, 2020. https://www.indiancountryecho.org
-
University of New Mexico. Our story. Project ECHO. Accessed September 1, 2020. https://echo.unm.edu/about-echo/model/
-
Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary Issues. Am J Public Health. 2014;104(suppl 3):S263-S267.
-
Tobey M, Armstrong K, Warne D. The 2019 partial government shutdown and its impact on health care for American Indians and Alaska Natives. J Health Care Poor Underserved. 2020;31(1):75-80.