Case
Mrs. McGoldrick was admitted to the local hospital from a local nursing home with a urinary tract infection (UTI) and multiple chronic diseases including diabetes and a history of heart attacks. Mrs. McGoldrick is 81 years old, has an adult daughter and an elderly sister. During the admission process, Mrs. McGoldrick reported that she could walk only with pain and therefore spent most of her day sitting in a chair. She was evaluated by a psychiatrist immediately after admittance and was prescribed antidepressants to combat symptoms of clinical depression. She was also observed to have indications of early stage dementia.
After spending 3 days in the hospital, Mrs. McGoldrick appeared to have been successfully treated for the UTI but remained weak and lethargic. In an effort to elevate her mood, the anti-depressant dosage was increased, but after several days there were no marked signs of improvement. One of the most distressing trends noted by the clinical staff was Mrs. McGoldrick's intake of foods and liquids. Several tests revealed that she was suffering from hypoprotein anemia which suggested that the she had not been properly nourished for a sustained period of time. The hospital staff, however, observed Mrs. McGoldrick eating and drinking well when her sister fed her during one of her regular visits.
Prior to Mrs. Goldrick's release from the hospital, her primary care physician, Dr. Misenti, spoke privately with Mrs. McGoldricks's daughter, who stated that her mother had expressed a "wish to die," believing that there was nothing more that she wanted from this life. After considering this information, Dr. Misenti suggested continuing the anti-depressants and giving Mrs. Goldrick the option of a percutaneous endoscopic gastrostomy (PEG), which might help raise her mood and nutritional status and, hence, her quality of life. It was Dr. Misenti's hope that by improving the quality of Mrs. McGoldrick's life, he would also encourage her to want to live. Her daughter believed that this was an idea that should be explored and implemented, but Mrs. McGoldrick refused to consider the option.
Commentary 3
The case of Mrs. McGoldrick stimulates us to think about the meaning of patient autonomy for a patient with cognitive impairment and about how surrogate decision makers should evaluate quality of life. Before we consider the ethical dimensions of the case, however, we must consider the medical aspects.
The first area that should be addressed is Mrs. McGoldrick's physical pain. We are told that her pain is severe enough to prevent her from walking and to confines her to a chair. It is essential to try to establish the etiology of the pain and to treat it vigorously. Pain control is the foundation of good palliative care, and lack of treatment may be at the heart of the patient's depressive symptoms and apparent lack of interest in life.1
The second domain that requires further exploration is Mrs. McGoldrick's depression. She was started on antidepressants at the time of admission to the hospital, and, when she remained weak and lethargic after 3 days, the dose was increased. Tricyclic antidepressants take 4-6 weeks to become effective; selective serotonin reuptake inhibitors typically require 2 weeks, and, while we are not told what medication is prescribed, almost all take longer than 3 days to work. If Mrs. McGoldrick's depression is contributing to her anorexia, then she should probably be treated with a stimulant such as methylphenidate. The dose can be increased rapidly, and, if the patient continues to have depression with life-threatening consequences, electroconvulsive therapy should be considered.
Third, the question of dementia ought to be further pursued. We are told that Mrs. McGoldrick has early dementia and, while truly reversible dementia is rare, it is important to rule out hypothyroidism and, especially in view of the patient's poor nutrition, pernicious anemia. If Mrs. McGoldrick has mild Alzheimer's disease, treatment with Donepezil should be considered. Although controversy persists over whether anti-cholinesterase inhibitors produce clinically meaningful benefits, if they have any role, it is in the early stages of Alzheimer's.2
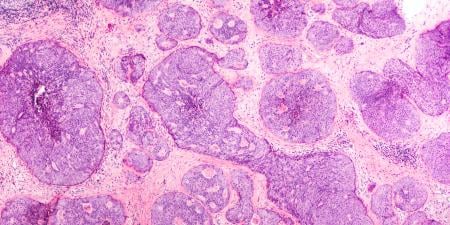
Finally, Mrs. McGoldrick's nutritional status warrants further examination. Her physician states that improved nutrition, delivered through a gastrostomy tube, will improve her quality of life and mood. While this assertion is intuitively appealing, there is little data to support the beneficial effect of artificial nutrition in the frail elderly: in a community study of 150 older individuals who received gastrostomy tubes, there was no improvement in health-related quality of life among those who survived more than 60 days.3 In the same study, there was no change in depression scores or functional status which might contribute to quality of life. Drawing inferences about the effects of gastrostomy tubes on quality of life from our intuition has proved hazardous in other, clinically distinct, situations such as that of patients with advanced dementia. In this setting, feeding tubes are often presumed to enhance quality of life by preventing aspiration pneumonia, improving function, and decreasing pressure ulcers, but in fact they have not been proven to reliably achieve any of these surrogate markers.4 While the role of artificial nutrition remains controversial, the only circumstances where there is consensus regarding benefit are isolated dysphagia and other non-progressive conditions that Mrs. McGoldrick does not manifest.5 The physician's suggestion that artificial nutrition would likely benefit Mrs. McGoldrick also fails to take into consideration such adverse consequences of a gastrostomy tube: diarrhea, infection, and the need for restraints if the patient tries to pull out the tube.
If, after the caregiving team responds to these unresolved medical problems, Mrs. McGoldrick continues to eat poorly and to express the wish to die, it is time to grapple with the ethical issues. Can the patient be compelled to accept a potentially life-saving intervention against her will? To answer this question, we must first ascertain whether Mrs. McGoldrick has decision-making capacity. The fact that she has mild cognitive impairment—assuming she has early dementia rather than delirium from her infection—does not necessarily mean that she is incapable of making decisions about a gastrostomy tube. She needs to be able to communicate her understanding of the nature of the proposed procedure, the alternatives to the procedure, and the consequences of both inserting and not inserting a gastrostomy tube.6 We do not have sufficient information about Mrs. McGoldrick to know whether she meets this standard. The effect of her depression on her ability to make decisions is also a concern. The presence of depression, however, does not automatically deprive a person of the ability to participate in his or her own medical care.7
Let us suppose that Mrs. McGoldrick has had her pain and depression vigorously and successfully addressed. Let us suppose, in addition, that her primary care physician and the consulting psychiatrist assess her to be incapable of making life and death decisions. When she is told that she might feel better—and feel differently about living longer—if she had a feeding tube, she just repeats that she doesn't want it and she does not seem to be able to process the possibility that she might have a new attitude towards life if her nutrition were improved (a claim which, as mentioned above, is entirely speculative and not grounded in any persuasive data). Under these circumstances can a surrogate decision maker authorize the intervention against her will?
One standard for determining whether a surrogate can demand an intervention that the patient opposes is a sliding scale of decision-making capacity.8 We commonly accept that a patient may refuse to have her blood drawn, even if she fails to fully understand the benefits of the test, because she does grasp its burdens and, at the same time, the test is very unlikely to be a matter of life and death. We also acknowledge that when a patient who is deemed incapable of making his own medical decisions and says he does not want a surgical intervention, but fails to understand that he will die without it, his decision can be overridden by his surrogate (assuming that the patient, when decision-capable, did not decline life-prolonging medical treatment). In the case of Mrs. McGoldrick, who says she doesn't want a gastrostomy tube but may not fully appreciate the consequences of the choice, the ultimate decision may be left to a surrogate if it has been formally established that the patient lacks the capacity to make her own decisions. The actual benefits of artificial nutrition are not well-established, the burdens are significant, and, most importantly, there is a less invasive alternative: the patient's sister, who has been successful in feeding her or coaxing her to eat, can be asked to play a more active role in her care. The patient's daughter can be recruited to share in caregiving tasks by visiting more regularly and providing greater support. The medical profession is often eager to find a quick fix; this is a situation that will take time to sort out. As Mrs. McGoldrick's depressive symptoms improve, as her pain resolves, as she engages in life review with a social worker or a chaplain, and as she spends more time socializing with her family—and eating as she socializes—perhaps her assessment of her quality of life will change. The medical team and Mrs. McGoldrick's family must avoid "conflating…the meaning of caring for the patient with the provision of a feeding tube."9
References
- Morrison RS, Meier DE. Clinical practice: palliative care. N Engl J Med. 2004;350(25):2582-2590.
-
Courtney C, Farrell D, Gray R, et al, for the AD2000 Collaborative Group. Long-term donepezil treatment in 565 patients with Alzheimer's disease (AD2000): randomized double-blind trial. Lancet. 2004;363(9427):2105-2115.
- Callahan CM. Outcomes of percutaneous endoscopic gastrostomy among older adults in a community setting. J Amer Geriatr Soc. 2000;48(9):1048-1054.
- Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia. A review of the evidence. JAMA. 1999;282(14):1365-1370.
- Rabeneck L, McCullough L, Wray N. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
- Appelbaum PS, Grisso J. Assessing patients' capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
- Blank K, Robison J, Doherty E, et al. Life-sustaining treatment and assisted death choices in depressed older patients. J Amer Geriatr Soc. 2001;49(2):153-161.
- Drane JF. Competency to give an informed consent. A model for making clinical assessments. JAMA. 1984;252(7):925-927.
-
Slomka J. What do apple pie and motherhood have to do with feeding tubes and caring for the patient? Arch Intern Med. 1995;155(12):1258-1263.