Abstract
Since the mid-1990s, poor oral health has been neglected as a public health threat, despite its recognition as epidemic in scale by the US Department of Health and Human Services Office of the Surgeon General. Americans’ poor oral health influences their overall health and, from a population standpoint, incurs dire economic and human costs. This article describes how health information transfer within the Marshfield Clinic Health System’s integrated medical and dental practice can improve diabetes care. This article also considers ethics and equity implications of improving MDP electronic health record interoperability in this large, rural Wisconsin organization.
Records and Equity
Chronic diseases are best managed by coordinating care, such that interventions are discussed within teams of cross-disciplinary clinicians and efficiently incorporated into service delivery, facilitating patients’ understanding of their options, care, and recovery plans. However, separate medical-dental service delivery streams and reimbursement systems and limited interprofessional training continue to undermine effective chronic disease management strategies.1,2,3 Oral health’s importance to general health is not routinely discussed in primary care settings, which results in missed research and patient education opportunities, prevention implementation, and dental referrals.4 Moreover, siloed medical and dental practice inequitably affects patients with chronic conditions, since separate storage and inadequate sharing of patients’ health records can compromise quality of care, especially during routine medical or dental appointments or emergency department visits.
This article describes the need for improved electronic health record (EHR) interoperability and how health information transfer within the Marshfield Clinic Health System’s integrated medical and dental practice can improve diabetes care.
Diabetes and Health Information Exchange
In 2000, the US Surgeon General recognized oral disease as a “silent epidemic”5 that increases morbidity and the economic burden of disease.6,7,8 Chronic oral diseases (eg, dental caries and periodontal disease) are linked to patients’ development of chronic diseases, such as diabetes.9,10 Total deaths in the United States due to diabetes is expected to increase by 38% between 2015 and 2030,11 and several dental diseases are common complications of diabetes.12 Periodontal disease interventions could lower annual costs for patients with type 2 diabetes, stroke, heart disease, and pregnancy and reduce inpatient admissions.13 Despite these benefits, geriatric, pediatric, low-income, uninsured, underinsured, and chronically ill patients are particularly likely to have their oral health needs underestimated or missed altogether by clinicians.14 One reason for these patients’ unmet oral health needs is that operable health information exchange (HIE) between medical and dental clinicians about such patients is nonexistent or inferior.15 The rest of this article is devoted to explaining why HIE is a patient-centered care practice that can improve patients’ outcomes and reduce health care utilization for patients with diabetes.16,17,18
The Institute for Electrical and Electronics Engineering defines interoperability as “the ability of two or more systems or components to exchange information and to use the information that has been exchanged.”19 To help promote interoperability and holistic patient care, the Institute of Medicine developed a list of health information technology (HIT) recommendations to support effective, efficient flow of patients’ health information across care settings.20 EHR integration promotes health equity by improving HIT interoperability and enabling secure HIE.21 Physical and virtual integration of organizations’ EHR infrastructure can generally be implemented in 1 of 3 ways:
- Ad hoc implementation: fully integrated medical-dental EHR architecture conforms to national standards.
- Broad implementation: EHR architecture supports interoperability within proprietary clinical information systems (eg, EPIC’s Wisdom module22).
- Universal implementation: EHR architecture supports interoperability across different clinical information systems (eg, regional HIE platforms).
Some organizations, such as the Marshfield Clinic Health System (MCHS), Kaiser Permanente, HealthPartners, and federally qualified health centers (FQHCs), have adopted and implemented virtual and physical EHR integration where dental and medical practices are geographically close in order to promote care continuity for patients, including those with diabetes.4
Establishing Interoperability
The MCHS was founded in 1916 as Marshfield Clinic and is one of the largest comprehensive integrated health systems in the United States.23,24 A multispecialty group and health professions learning environment, MCHS serves communities in health professional shortage areas25 and patients living in central, western, and northern regions of Wisconsin and in Michigan’s Upper Peninsula.26 In the early 2000s, oral health services access for rural Medicare- and Medicaid-eligible patients was substantially limited. Family Health Center (FHC), an FQHC that has served low-income, underinsured, and uninsured patients since 1974, partnered with MCHS in 2002 to establish a dental safety net. Ten dental care sites now serve more than 50 000 unique patients annually,24 regardless of income or insurance status, with a goal of mitigating health inequity (see Table).
| Year | |||
|---|---|---|---|
| Insurance Type | 2017 | 2018 | 2019 |
| Commercial, no. (%) | 11 980 (20.04%) | 12 559 (21.44%) | 12 781 (22.60%) |
| Medicaid, no. (%) | 37 716 (63.09%) | 36 571 (62.11%) | 34 769 (61.49%) |
| Self-pay, no. (%) | 4869 (8.14%) | 4728 (8.03%) | 4634 (8.19%) |
| Sliding Fee Scale, no. (%) | 5213 (8.72%) | 5018 (8.52%) | 4354 (7.70%) |
| Total | 59 778 | 58 876 | 56 538 |
| aData from Marshfield Clinic Health System enterprise data warehouse. | |||
Although MCHS services are supported by a customized medical-dental integrated EHR (iEHR),23,24 barriers to medical-dental care integration for patients with diabetes remained and were further studied. Based on 2018-2019 aggregate EHR data, 8% of MCHS medical and dental patients (6363 of 71 811) were diagnosed with diabetes. Approximately 7% of patients diagnosed with diabetes (32 131 of 472 591) only visited MCHS medical, but not dental, centers. With these data in mind, investigators first sought to understand perceived practice gaps and barriers to medical-dental integration.27,28 Surveys2,3,29 and focus groups were conducted with MCHS/FHC medical and dental clinicians to assess their knowledge of, attitudes toward, and practice of integrated care.2,3,29,30 Participants’ responses informed development of educational tools for clinicians and patients, informed which metrics would be used to assess these tools’ efficacy, and led to incorporating a clinical decision support alert tool (CDSAT) into practice to help diagnose patients with diabetes.
Figure. Screenshot of the Clinical Decision Support Alert Tool Used at Marshfield Clinic Health System
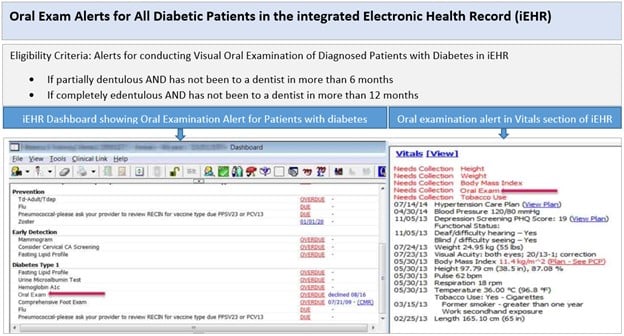
© Marshfield Clinic Health System (MCHS), Inc. All rights reserved. Reprinted with permission of MCHS.
Eligibility criteria in the CDSAT of a patient’s iEHR alert primary care clinicians to conduct visual oral examinations of patients with diabetes. Four years after the CDSAT was implemented in 2014 at 2 pilot MCHS medical sites, evaluation of the CDSAT revealed that it triggered a total of 7723 patients’ EHRs to issue an alert. In response to alerts, primary care clinicians visually orally examined 4943 patients with diabetes (64%); among those patients, 170 were referred to dentists and 626 were advised to visit a dentist. Additionally, another study developed risk assessment tools using informatics techniques. Since informatics tools help predict diabetes risk among patients in dental settings,31 the study team screened patients for risk of diabetes using machine-learning techniques that extracted medical-dental variables from the iEHR. Using this predictive tool in MCHS dental centers enabled patients at risk for developing diabetes to be identified by dentists, who then referred them to physicians.
Next Steps
Centers for Medicaid and Medicare Services data indicate that MCHS was the most successful participant in a 2011 Physician Group Practice demonstration project, as it earned 57% of the $107.6 million in gross savings realized over a 5‐year period, most of which was distributed among the 10 participating MCHS institutions based on performance.32 Outcomes of the demonstration project validated that integrating medical and dental care, supported by use of informatics and quality tracking, delivered high-quality care at reduced cost.32 Subsequent research and quality improvement projects have also demonstrated improvements in health care outcomes, patient safety, and patient satisfaction.26,27,28,33 While medical-dental HIE is the focus of this case study, integrated care, according to the World Health Organization, is about patients’ experiences—specifically, about “the organization and management of health services so that people get the care they need, when they need it, in ways that are user-friendly, achieve the desired results and provide value for money.”34 Integrated service delivery facilitated by HIE also nourishes professional ethics and health equity.35,36,37
MCHS/FHC established medical-dental interoperability, via EHR integration, to identify diabetic and prediabetic patients in predominantly rural areas of Wisconsin and Michigan and to facilitate such patients’ access to prevention and management interventions. Integrated care holds promise for alleviating health inequities, specifically for rural populations. President Joseph Biden has been pressured to appoint a rural health “czar,”38 and medical-dental integration successes of the MCHS/FHC model could be replicated in other US regions and for other chronic disease states.
References
-
Harnagea H, Couturier Y, Shrivastava R, et al. Barriers and facilitators in the integration of oral health into primary care: a scoping review. BMJ Open. 2017;7(9):e016078.
- Shimpi N, Schroeder D, Kilsdonk J, et al. Medical providers’ oral health knowledgeability, attitudes, and practice behaviors: an opportunity for interprofessional collaboration. J Evid Based Dent Pract. 2016;16(1):19-29.
- Shimpi N, Jurich I, Panny A, Acharya A. Knowledgeability, attitude, and practice behaviors of primary care providers toward managing patients’ oral health care in medical practice: Wisconsin statewide survey. J Am Dent Assoc. 2019;150(10):863-872.
-
Atchison KA, Rozier RG, Weintraub JA. Integration of oral health and primary care: communication, coordination and referral. NAM Perspect. October 8, 2018. Accessed November 10, 2021. https://nnoha.org/nnoha-content/uploads/2019/12/Integration-of-Oral-Health-and-Primary-Care.pdf
-
US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. Accessed November 8, 2021. https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf
- Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. J Periodontol. 2006;77(9):1465-1482.
- DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM. Dental disease and risk of coronary heart disease and mortality. BMJ. 1993;306(6879):688-691.
- Petersen PE, Ogawa H. The global burden of periodontal disease: towards integration with chronic disease prevention and control. Periodontol 2000. 2012;60(1):15-39.
- Mealey BL. Periodontal disease and diabetes. A two-way street. J Am Dent Assoc. 2006;137(suppl):26S-31S.
-
Shimpi N, Ashton J, Sorenson C, et al. Interdisciplinary care model: diabetes and oral health. In: Acharya A, Powell V, Torres-Urquidy M, Posteraro R, Thyvalikakath T, eds. Integration of Medical and Dental Care and Patient Data. 2nd ed. Springer Nature; 2019:47-61.
- Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: insights from yesterday, today, and future trends. Popul Health Manag. 2017;20(1):6-12.
-
Diabetes, gum disease and other oral health problems. National Institute of Diabetes and Digestive and Kidney Diseases. Reviewed September 2014. Accessed June 20, 2021. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/gum-disease-dental-problems
- Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med. 2014;47(2):166-174.
-
Vulnerable populations: who are they? Am J Manage Care. 2006;12(13)(suppl):S348-S352.
- Simon L, Obadan-Udoh E, Yansane AI, et al. Improving oral-systemic healthcare through the interoperability of electronic medical and dental records: an exploratory study. Appl Clin Inform. 2019;10(3):367-376.
-
Hughes RG. Tools and strategies for quality improvement and patient safety. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality; 2008:chap 44.
- Greene SM, Tuzzio L, Cherkin D. A framework for making patient-centered care front and center. Perm J. 2012;16(3):49-53.
-
Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; 2001.
-
Fridsma D. Interoperability vs health information exchange: setting the record straight. Health IT Buzz blog. January 9, 2013. Accessed January 16, 2021. https://www.healthit.gov/buzz-blog/meaningful-use/interoperability-health-information-exchange-setting-record-straight
-
Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. National Academies Press; 2013.
-
21st Century Cures Act, HR 34, 114 Cong, 2nd Sess, §4003 (2016). Accessed February 20, 2021. https://www.congress.gov/114/bills/hr34/BILLS-114hr34enr.pdf
-
Software. Epic. Accessed February 20, 2021. https://www.epic.com/software
- Shimpi N, Ye Z, Koralkar R, et al. Need for diagnostic-centric care in dentistry: a case study from the Marshfield Clinic Health System. J Am Dent Assoc. 2018;149(2):122-131.
- Acharya A. Marshfield Clinic Health System: integrated care case study. J Calif Dent Assoc. 2016;44(3):177-181.
- Nycz G, Shimpi N, Glurich I, et al. Positioning operations in the dental safety net to enhance value-based care delivery in an integrated health-care setting. J Public Health Dent. 2020;80(suppl 2):S71-S76.
-
Shimpi N, Glurich I, Acharya A. Integrated care case study: Marshfield Clinic Health System. In: Acharya A, Powell V, Torres-Urquidy MH, Posteraro RH, Thyvalikakath T, eds. Integration of Medical and Dental Care and Patient Data. 2nd ed. Springer Nature; 2019:315-326.
- Acharya A, Shimpi N, Mahnke A, Mathias R, Ye Z. Medical care providers’ perspectives on dental information needs in electronic health records. J Am Dent Assoc. 2017;148(5):328-337.
- Glurich I, Schwei KM, Lindberg S, Shimpi N, Acharya A. Integrating medical-dental care for diabetic patients: qualitative assessment of provider perspectives. Health Promot Pract. 2018;19(4):531-541.
- Shimpi N, Schroeder D, Kilsdonk J, Chyou PH, Glurich I, Acharya A. Assessment of dental providers’ knowledge, behavior and attitude towards incorporating chairside screening for medical conditions: a pilot study. J Dent Oral Care Med. 2016;2(1):1-7.
- Shimpi N, Glurich I, Schroeder D, Katrak C, Chyou P-H, Acharya A. Patient awareness of association of diabetes and periodontal disease. Health Promot Pract. 2020;21(3):464-472.
-
Hegde H, Shimpi N, Panny A, Glurich I, Christie P, Acharya A. Development of non-invasive diabetes risk prediction models as decision support tools designed for application in the dental clinical environment. Inform Med Unlocked. 2019;17:100254.
-
Kautter J, Pope GC, Leung M, et al. Evaluation of the Medicare Physician Group Practice Demonstration. Centers for Medicare and Medicaid Services; 2012. Accessed November 11, 2021. https://downloads.cms.gov/files/cmmi/medicare-demonstration/PhysicianGroupPracticeFinalReport.pdf
-
Shimpi N, Hegde H, Glurich I, Ryan M, Acharya A. Establishing a quality improvement culture within a large integrated medical-dental health system with a population based focus. J Evid Based Dent Pract. Published online June 18, 2021.
-
World Health Organization. Integrated health services—what and why? May 2008. Accessed November 11, 2021. https://www.who.int/healthsystems/technical_brief_final.pdf
-
McKeown A, Cliffe C, Arora A, Griffin A. Ethical challenges of integration across primary and secondary care: a qualitative and normative analysis. BMC Med Ethics. 2019;20:42.
- Hodgson J, Mendenhall T, Lamson A. Patient and provider relationships: consent, confidentiality, and managing mistakes in integrated primary care settings. Fam Health. 2013;31(1):28-40.
-
Raus K, Mortier E, Eeckloo K. The patient perspective in health care networks. BMC Med Ethics. 2018;19:52.
-
Crampton L. American’s rural crisis triggers calls for Biden to name rural czar. Politico. January 25, 2021. Accessed June 21, 2021. https://www.politico.com/news/2021/01/25/america-rural-economy-health-biden-czar-461326



