Abstract
Limited understanding of public health disease prevention programs often leads to resistance, which ultimately results in low vaccine uptake. This article suggests how public health practitioners can improve public understanding of cervical cancer and HPV vaccination programs, which is key to improving health literacy, using culturally appropriate materials and approaches to boost public acceptance of vaccine programs.
Case
Dr M was trained in the United States but has returned to her native country to serve as the chief medical officer of a regional health district. This low-income country’s Ministry of Health has decided to fund human papillomavirus (HPV) vaccinations in Dr M’s district, given the recent increase of cervical cancer incidence. Understanding of HPV and cervical cancer is almost nonexistent in Dr M’s district, and she is extremely concerned about how to discuss risks and benefits of vaccination and obtain informed consent from parents of the 9- to 14-year-old girls. Dr M greets a girl’s mother, Ms A, at a district health center and begins to counsel Ms A about the HPV vaccine and cancer prevention. Ms A listens attentively and then asks in English, “Are you saying this cancer is an infection like HIV?” Dr M responds, “The cancer is caused by an infection, a virus. HIV is also a virus. But this vaccine protects you from HPV, not HIV.” Dr M attempts to clarify, but Ms A doesn’t appear convinced. “And this cancer, it grows in her belly, like a pregnancy? So, this vaccine will be like preventing pregnancy?” Dr M wonders which source of confusion to address first and then explains, “The vaccine will not affect whether she can have a family.” Ms A wonders, “If I say no to this vaccine, the cancer will grow, and she will not have children?” Dr M wonders how to respond.
Commentary
This case is a common one in low-income countries whose public health and health care delivery systems are dependent on foreign-trained practitioners. The challenges associated with the implementation of public health prevention programs in low-income countries go beyond patient-clinician communication. This commentary investigates how vaccine campaigns should balance ethical demands to clearly communicate risks and benefits with clinical and public health demands to efficiently administer large-scale programs. Using examples from some of our work conducted in an HIV prevention study setting in Malawi, we provide some suggestions for how clinicians and public health practitioners can improve public understanding of cancer prevention programs, with a focus on improving stakeholder engagement and health literacy.
Limited Understanding
Community members in low-income regions might have limited health literacy. Some might lack adequate vocabulary to describe either a specific disease or vaccines, and there can be confusion about disease causation.1,2 Nevertheless, lack of knowledge of a specific disease and of a vaccine for that disease should not be taken to imply that there are no cases of that disease in a region or that community members have no experiences with vaccination or other prevention strategies. Community members might simply view disease causation differently.3 For example, some might believe that a disease caused by a virus is instead caused by witchcraft.
Public health practitioners’ awareness of and capacity to disarm rumored misinformation is critical to the success of public health interventions.
Conversely, those implementing public health programs might lack knowledge of community members’ understanding of disease. Because they might not understand local traditions or appreciate their importance and impact, some public health professionals might fail to engage with community members in ways that facilitate local uptake of prevention programs or awareness of their importance. Lack of engagement might also be due to limited financial, personnel, or training resource investment in a public health intervention; a fundamental need for speedy public health intervention implementation,4 and to overemphasis on boosting numbers of patients vaccinated or insufficient respect for patients’ or parents’ rights to make decisions about whether to accept or reject an intervention for themselves or a child.5,6
Communication Goals
In many low- and middle-income regions, limited understanding or lack of knowledge of cervical cancer and prevention can interfere with vaccination uptake.7 Refusal or hesitancy to vaccinate one’s child against measles in the United States is one example.8 If disease prevention programs do not facilitate adequate explanation of an intervention’s benefits9 or overemphasize an intervention’s potential harms as a way to manage litigation risk, even patients or parents with high health literacy might refuse an intervention. Acceptance of any intervention depends on understanding not only risks and benefits but also the problem being addressed, why a proposed intervention is a useful solution, and the implications of the proposed intervention. Accordingly, acceptance of an HPV vaccine requires understanding cervical cancer and its associated risks, understanding the need for vaccination, understanding the risks and benefits of vaccination, and—more importantly—understanding the implications of present and future implications of vaccinating children before they’re sexually active. In the case, Dr M and fellow practitioners need to balance an ethical imperative to communicate clearly with community members about cervical cancer and the potential risks and benefits of vaccination with public health demand for efficient intervention. An efficiently implemented, administered, and executed vaccine campaign begins by promoting uptake in communities.
Engaging Community Members
Public health practitioners need to become familiar with how patients’ cultural and religious beliefs, for example, inform or obstruct their understanding of cervical cancer and HPV vaccines.1,10 In particular, clinicians and health educators from resource-rich regions should be aware of how their relative power and authority is perceived and experienced by those whom they seek to serve and should consider how to express respect for individuals’ self-determination in the context of community.11 It is particularly critical to express respect when discussing beliefs about disease causation that are “wrong” from an allopathic perspective, since a key to intervention uptake is making patients and community members allies in the overall public health effort. In the case, expressing respect for the region’s cultural and religious values would mean ensuring that women public health practitioners are the ones who interact with, and introduce the program to, local girls and their mothers.
Navigating Cultural Pluralism While Cultivating Common Need
One way to help ensure that community members start to feel the need for cervical cancer vaccination is to facilitate their understanding of cervical cancer’s regional severity and incidence. In the case, Dr M and fellow clinicians can focus on helping community members understand HPV vaccination as a way to preserve girls’ and women’s lives. Some might argue that it is only fair to extend vaccination to boys as well, since they are the ones who transmit the virus to girls during sexual intercourse. In some regional religious groups, sex is permitted only in marriage and some might fear that vaccinating children constitutes an endorsement of premarital sex. But Dr M and colleagues can perhaps draw upon regional marital and family-oriented values to problematize health beliefs that are wrong from an allopathic standpoint and to motivate the public health interests of children today, who might be the adult regional family leaders of tomorrow.
Disarming Misinformation, Improving Understanding
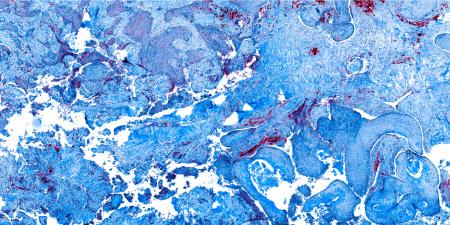
Low levels of health literacy can exacerbate language barriers and frustrate communication about risks and benefits of an intervention. When critical information about an intervention is not well understood by those who bear the risk of receiving it, gaps in understanding can be filled by misinformation and spread as rumor. Public health practitioners’ awareness of and capacity to disarm rumored misinformation is critical to the success of public health interventions.5,12,13 Furthermore, some languages do not have English-equivalent words14 to accurately describe cervical cancer, symptoms, treatments, or vaccines from an allopathic perspective. In such cases, public health practitioners and clinicians can use visuals to clearly describe cervical cancer and stories from everyday life to explain vaccinology. In Malawi, for example, agricultural pictures are used to try to explain placebos, double blinds, and randomization15,16 and lay language is used to facilitate a prospective research subject’s consent to enroll in a trial.17,18
When explaining HPV vaccination, public health practitioners must clearly describe a vaccine’s prospective short-term and long-term reproductive health risks and benefits or, if a vaccine is experimental, its risks and possible benefits. Some individuals might be familiar with vaccinations for diseases such as measles and tetanus that have been administered in low-income regions of the world in recent decades. If so, clinicians can draw upon known examples to help community members understand how mortality from these diseases was reduced by vaccine programs and to suggest reasons to hope for mortality reductions of an HPV vaccine.
References
- Dixey RA. “Fatalism,” accident causation and prevention: issues for health promotion from an exploratory study in a Yoruba town, Nigeria. Health Educ Res. 1999;14(2):197-208.
- Lykins EL, Graue LO, Brechting EH, Roach AR, Gochett CG, Andrykowski MA. Beliefs about cancer causation and prevention as a function of personal and family history of cancer: a national, population‐based study. Psychooncology. 2008;17(10):967-974.
- Bingham A, Drake JK, LaMontagne DS. Sociocultural issues in the introduction of human papillomavirus vaccine in low-resource settings. Arch Pediatr Adolesc Med. 2009;163(5):455-461.
- Streefland PH. Public doubts about vaccination safety and resistance against vaccination. Health Policy. 2001;55(3):159-172.
- Kaler A. Health interventions and the persistence of rumour: the circulation of sterility stories in African public health campaigns. Soc Sci Med. 2009;68(9):1711-1719.
-
World Health Organization. Immunization in Practice: A Practical Guide for Health Staff. https://apps.who.int/iris/bitstream/handle/10665/193412/9789241549097_eng.pdf;jsessionid=BD3489C2397C90BB929322C1B3B73445?sequence=1. Published 2015. Accessed December 6, 2019.
-
Chidyaonga-Maseko F, Chirwa ML, Muula AS. Underutilization of cervical cancer prevention services in low and middle income countries: a review of contributing factors. Pan Afr Med J. 2015;21:231.
- Sarkar S, Aleksa Z, Kamran K, Gardner L. Measles resurgence in the USA: how international travel compounds vaccine resistance. Lancet Infect Dis. 2019;19(7):684-686.
- Gostin LO. Law, ethics, and public health in the vaccination debates: politics of the measles outbreak. JAMA. 2015;313(11):1099-1100.
- Stanton BF. Assessment of relevant cultural considerations is essential for the success of a vaccine. J Health Popul Nutr. 2004;22(3):286-292.
- Padela AI, Malik AY, Curlin F, De Vries R. [Re]considering respect for persons in a globalizing world. Dev World Bioeth. 2015;15(2):98-106.
- Dodoo A, Adjei S, Couper M, Hugman B, Edwards R. When rumours derail a mass deworming exercise. Lancet. 2007;370(9586):465-466.
- Ghinai I, Willott C, Dadari I, Larson HJ. Listening to the rumours: what the northern Nigeria polio vaccine boycott can tell us ten years on. Glob Public Health. 2013;8(10):1138-1150.
- Cornelli AC, Bentley ME, Sorenson JE, Henderson GE. Using formative research to develop a context-specific approach to informed consent for clinical trials. J Empir Res Hum Res Ethics. 2006;1(4):45-60.
-
Ndebele PM, Wassenaar D, Munalula E, Masiye F. Improving understanding of clinical trial procedures among low literacy populations: an intervention within a microbicide trial in Malawi. BMC Med Ethics. 2012;13(1):29.
- Ndebele P, Wassenaar D, Masiye F, Munalula-Nkandu E. Trial participants’ understanding of randomization, double-blinding, and placebo use in low literacy populations: findings from a study conducted within a microbicide trial in Malawi. J Empir Res Hum Res Ethics. 2014;9(3):2-10.
-
Cornelli A, Sorenson J, Bentley M, et al; Breastfeeding, Antiretroviral, and Nutrition Informed Consent Group. Improving participant understanding of informed consent in an HIV-prevention clinical trial: a comparison of methods. AIDS Behaviour. 2012;16(2):412-421.
-
Mandava A, Pace C, Campbell B, Emanuel E, Grady C. The quality of informed consent: mapping the landscape. A review of empirical data from developing and developed countries. J Med Ethics. 2012;38(6):3.