Abstract
Cancer care in low-resource regions is complex, as resources and infrastructure for cancer care and prevention are limited. Mortality rates for breast cancer in particular are higher in regions where treatments are unavailable, unaffordable, or cost ineffective. Clinical breast examination is a reasonable screening approach, although its effects on mortality have not yet been shown. This article recommends focusing on early detection of symptomatic disease (ie, downstaging) and treatment of early detected breast cancers with potentially curative strategies.
Case
Ms P, a 59-year-old woman who lives in a remote, low-income region, has worried about cancer ever since her mother died from metastatic breast cancer a year ago. As the family’s sole income earner, she would not be able to support her children if she developed a serious illness. When visiting Dr A for her child’s earache, she tells Dr A that she wishes she could get a mammogram so that any cancer could be detected and treated early.
There are only 2 clinics in the country where mammography is available, and Ms P has access to neither without making a long journey that she cannot afford. However, Dr A does have an ultrasound machine. Although ultrasound is generally not accepted as a way to screen for breast cancer,1 Dr A has experience using ultrasound in a variety of diagnostic and screening contexts,1 and perhaps using it would ease Ms P’s mind. Dr A wonders whether to offer to examine Ms P via ultrasound.
Commentary
The global burden of cancer—including breast cancer—is growing, with low-income countries (LICs) contributing to the majority of new breast cancer cases and deaths.2,3 Indeed, LICs now contribute to roughly 53% of global breast cancer incidence.3 In addition, because the resources and infrastructure for cancer care and control are limited in LICs relative to high-income countries (HICs), the mortality rates for breast cancer are higher in LICs.4 In fact, breast cancer remains the number one cancer killer among women in LICs.3 Thus, the patient described in the vignette is appropriately concerned about her risk of breast cancer and her likely outcome, given that she resides in an LIC. However, whether screening is the appropriate solution remains a challenging question.
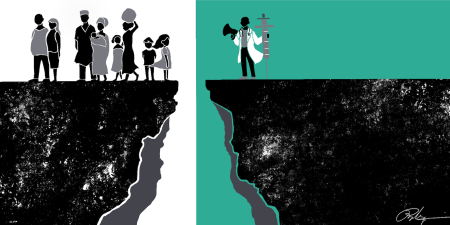
Screening for breast cancer in LICs presents a paradoxical dilemma. On the one hand, no screening would lead to increased odds of presentation at advanced-stage disease for which treatments are unavailable, unaffordable, and cost ineffective. On the other hand, LICs are not equipped to both implement a screening campaign effectively and deal with the downstream consequences of screening-detected lesions, most of which end up not being cancer.5 Debate persists even about whether mammography screening is appropriate in HICs.6 The United States Preventive Services Task Force (USPSTF) assigns a grade B recommendation for biennial mammogram screening for women aged 50 to 74 who are not at high risk.7 (The USPSTF recommendation grades range from A (highest) to D (lowest), where grade B implies recommended service based on high certainty of moderate benefit or moderate certainty of moderate to substantial benefit.8) For the sake of discussion, let’s assume this recommendation applies to women in LICs. Since Ms P is in this age group, should mammography screening be recommended, despite not being locally available? And should ultrasound screening be offered instead because she can’t afford the journey for a mammogram? If neither is appropriate, what alternatives are there for Ms A’s care?
Mammography in LICs
For screening to be appropriate, it “must be acceptable, equitable, accessible, sustainable, and economically efficient for the target population.”9 The aim of a screening campaign for cancer thus could be different in low- and middle-income countries vs HICs. In resource-poor settings, focusing on mitigating symptomatic disease should be prioritized rather than, as in developed nations, focusing on cancer detection in asymptomatic women. For example, a cohort study from Uganda revealed that 77% of breast cancer patients at a national cancer hospital had advanced disease, defined as stage III or IV.10 Thus, LICs should focus more on reducing advanced-stage diagnoses by using campaigns to educate women and to encourage symptomatic women to come forward for diagnostic evaluation. For Ms P, living in an LIC, tumor detection at the earliest stage should be the clinical and ethical priority.
If appropriate clinical care for a detected lesion is unavailable, one could argue that it’s not ethically justifiable to screen without capacity to treat.
An important aspect of the debate about cancer screening in LICs is the effect of screening on all-cause mortality vs cancer mortality. For example, although mammography reduces breast cancer-related deaths among women in Ms P’s age group,11 overall life expectancy for women in LICs is less than that of HICs.12 The upshot here is that, while it is important to address Ms P’s concerns, it is also important to consider that screening mammography has failed to improve all-cause mortality, even in HICs.13
If we consider the costs, inconvenience, and inaccessibility of mammography in LICs, together with the infrastructure needed to implement it, there is arguably less justification to spend limited resources for this screen, given its limited evidence of effectiveness and potential for harm. In sum, the inconvenience of a mammogram could be justified for diagnostic purposes if Ms P has symptoms, but probably not for screening.
Ultrasound in LICs
In general, as mentioned in the case, ultrasound is not recommended as a screening modality. Even when ultrasound is used as an adjunct to mammography, its effect on reducing breast-cancer mortality is uncertain, and screening with adjunct ultrasound actually increases false positives in women at high risk.14
For Ms P, there is a small chance that ultrasound would be helpful and a risk of harm of a false positive.
However, in deciding whether to offer Ms P ultrasound, we need to consider not only the evidence but also the economic context. Screening is not a one-time detection intervention; for a screening program to function well and be clinically and ethically justifiable, resources must be sufficient to respond to the downstream follow-up required for patients in whom a lesion is detected, including referral, confirmation diagnostics, and treatment. If Ms P’s local center doesn’t have mammography, it probably doesn’t have sufficient resources for biopsy, surgery, radiation, and other procedures. Given the lack of follow-up capacity, the risk of harm from a false positive should be regarded as clinically and ethically prominent.
Previous cost-effectiveness studies suggest that treating stage I breast cancer is the best breast cancer control strategy for LICs.15,16 Ideally, all cases of breast cancer would be discovered early and referred to a surgeon. However, many LICs lack surgery, pathology, and radiation facilities. Nearly 80% of patients in LICs require surgical oncologic care, but 75% will not have timely access.17 Other studies similarly show that women in LICs lack access to appropriate pathology and radiotherapy services.15,18,19 How, then, should we advocate and care for patients like Ms P?
The goal of screening is not just to detect but to treat detected disease.6,20 For Ms P, diagnosis and treatment will remain challenges, so is it ethically appropriate to pursue tumor detection if treatment is not available to her? A breast cancer diagnosis could cause distress, physical harm, and unknown downstream consequences. If appropriate clinical care for a detected lesion is unavailable, one could argue that it’s not ethically justifiable to screen without capacity to treat.
Screening for Asymptomatic Disease vs Early Detection of Symptomatic Disease
Diagnostic delay is an important cause of late-stage diagnosis for women in LICs. Previous studies have evaluated patient delays (lag from initial symptoms to presentation to a clinician) and clinician delays (lag from a patient’s first presentation to diagnosis or treatment).21,22,23,24,25 Patient delay can be due to a patient’s lack of awareness of breast cancer symptoms, severity of disease progression, lack of access to a qualified clinician, or lack of financial means to pay for treatment.24,25,26,27,28 Lack of breast cancer experience and knowledge among primary care clinicians and quality deficiencies in cancer care contribute to clinician delays in LICs, although this topic has been less extensively investigated.27 We recommend as a national screening strategy that LICs prioritize early detection among patients with symptomatic disease to help reduce the kinds of delays just described. Interventions to reduce delays in care would increase the number of patients with potentially curable breast cancer who seek care and reduce breast cancer mortality while minimizing expenditure of limited resources. To address the needs of women like Ms P and the population needs of LICs, clinical breast examination (CBE) could be a reasonable middle-ground approach.6
Many women with breast cancer in LICs seek care when their cancers have progressed beyond curability.29 Treating advanced disease is less hopeful and more expensive and requires complex infrastructure and the availability of multiple subspecialties. By contrast, treating women whose breast cancers are detected early can be done with less costly surgery, radiotherapy, and limited-time adjuvant treatment. CBE has been proposed by the International Agency for Research on Cancer as an alternative to mammography to detect breast cancers at an earlier stage.30 In Malaysia, for example, there was a 41.7% reduction in the proportion of patients presenting with advanced-stage breast cancer within 5 years of introducing a cancer surveillance program that included CBE screening.29 In Indonesia, CBE was nearly as effective as mammography,31 and, in India, annual CBE was estimated to be as effective as mammography but only half the cost.32,33 Because detecting cancer at an early stage when treatment is more affordable is important for LICs, CBE can be an important tool of cancer control in LICs if implemented properly.
For Ms P, CBE would likely be more appropriate than mammography. Preliminary data from trials in low-income settings suggest that CBE screening can lead to downstaging of breast cancer, although its effect on mortality hasn’t been shown.34,35 Because a substantial proportion of women in LICs present with late-stage breast cancer,29,36 for women like Ms P and others in LICs, downstaging is critical.
Recommendations
The feasibility of CBE has been established in LICs.35,37 Our argument is not that CBE is a good screening tool but that it is a more pragmatic choice than mammography in LICs. For screening programs to be effective and affordable, high-quality treatment must be available. Accordingly, socioeconomic and other barriers to treatment should be addressed as part of cancer control policy in LICs. In addition, what needs to be available are good pathology, surgery and radiotherapy, supportive care services, surveillance and monitoring systems, and a cancer registry. Screening without good follow-up care across the cancer continuum makes little clinical or ethical sense, as one could argue that resources devoted to breast cancer screening would be better spent on public and professional education such as tobacco cessation, alcohol control, and healthy diet and lifestyle promotion. We propose that health services in low-resource regions test CBE in a small district and monitor the program’s feasibility, acceptability, effectiveness, and cost.
References
- Omidiji OA, Campbell PC, Irurhe NK, Atalabi OM, Toyobo OO. Breast cancer screening in a resource poor country: ultrasound versus mammography. Ghana Med J. 2017;51(1):6-12.
-
World Health Organization. Breast cancer: prevention and control. https://www.who.int/cancer/detection/breastcancer/en/index1.html. Accessed November 18, 2019.
-
GLOBOCAN 2018: counting the toll of cancer [editorial]. Lancet. 2018;392(10152):985.
-
American Cancer Society. Global cancer: facts & figures. 3rd ed. https://documentcloud.adobe.com/link/track?uri=urn%3Aaaid%3Ascds%3AUS%3A4dcd11b8-b10c-46d2-b3ee-a938da3747f5. Published 2015. Accessed November 18, 2019.
- Vizcaino I, Gadea L, Andreo L, et al. Short-term follow-up results in 795 nonpalpable probably benign lesions detected at screening mammography. Radiology. 2001;219(2):475-483.
-
Gyawali B, Shimokata T, Honda K, Tsukuura H, Ando Y. Should low-income countries invest in breast cancer screening? Cancer Causes Control. 2016;27(11):1341-1345.
-
US Preventive Services Task Force. Final recommendation statement, breast cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening1. Published January 2016. Accessed October 30, 2019.
-
US Preventive Services Task Force. Grade definitions. https://www.uspreventiveservicestaskforce.org/Page/Name/grade-definitions. Updated June 1, 2018. Accessed November 18, 2019.
-
Shah SC, Kayamba V, Peek RM, Heimburger D. Cancer control in low-and middle-income countries: is it time to consider screening? J Glob Oncol. 2019;5:1-8.
- Gakwaya A, Kigula-Mugambe JB, Kavuma A, et al. Cancer of the breast: 5-year survival in a tertiary hospital in Uganda. Br J Cancer. 2008;99(1):63-67.
- Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599-1614.
-
Bellanger M, Zeinomar N, Tehranifar P, Terry MB. Are global breast cancer incidence and mortality patterns related to country-specific economic development and prevention strategies? J Glob Oncol. 2018;4:1-16.
- Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 US Preventive Services Task Force recommendation. Ann Intern Med. 2016;164(4):244-255.
- Health Quality Ontario. Ultrasound as an adjunct to mammography for breast cancer screening: a health technology assessment. Ont Health Technol Assess Ser. 2016;16(15):1-71.
- Gelband H, Sankaranarayanan R, Gauvreau CL, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387(10033):2133-2144.
- Groot MT, Baltussen R, Uyl-de Groot CA, Anderson BO, Hortobagyi GN. Costs and health effects of breast cancer interventions in epidemiologically different regions of Africa, North America, and Asia. Breast J. 2006;12(suppl 1):S81-S90.
- Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16(11):1193-1224.
- Farmer P, Frenk J, Knaul FM, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet. 2010;376(9747):1186-1193.
- Rodin D, Jaffray D, Atun R, et al. The need to expand global access to radiotherapy. Lancet Oncol. 2014;15(4):378-380.
- Gyawali B. Me, too. J Glob Oncol. 2016;2(3):99-104.
- Chalkidou K, Marquez P, Dhillon PK, et al. Evidence-informed frameworks for cost-effective cancer care and prevention in low, middle, and high-income countries. Lancet Oncol. 2014;15(3):e119-e131.
- Unger-Saldana K. Challenges to the early diagnosis and treatment of breast cancer in developing countries. World J Clin Oncol. 2014;5(3):465-477.
-
Sharma K, Costas A, Shulman LN, Meara JG. A systematic review of barriers to breast cancer care in developing countries resulting in delayed patient presentation. J Oncol. 2012;2012:121873.
- Otieno ES, Micheni JN, Kimende SK, Mutai KK. Provider delay in the diagnosis and initiation of definitive treatment for breast cancer patients. East Afr Med J. 2010;87(4):143-146.
- Clegg-Lamptey J, Dakubo J, Attobra YN. Why do breast cancer patients report late or abscond during treatment in Ghana? A pilot study. Ghana Med J. 2009;43(3):127-131.
- Ibrahim NA, Oludara MA. Socio-demographic factors and reasons associated with delay in breast cancer presentation: a study in Nigerian women. Breast. 2012;21(3):416-418.
- Pace LE, Mpunga T, Hategekimana V, et al. Delays in breast cancer presentation and diagnosis at two rural cancer referral centers in Rwanda. Oncologist. 2015;20(7):780-788.
- Ukwenya AY, Yusufu LM, Nmadu PT, Garba ES, Ahmed A. Delayed treatment of symptomatic breast cancer: the experience from Kaduna, Nigeria. S Afr J Surg. 2008;46(4):106-110.
- Devi BC, Tang TS, Corbex M. Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak, Malaysia. Ann Oncol. 2007;18(7):1172-1176.
- Lauby-Secretan B, Loomis D, Straif K. Breast-cancer screening—viewpoint of the IARC Working Group. N Engl J Med. 2015;372(24):2353-2358.
- Kardinah D, Anderson BO, Duggan C, Ali IA, Thomas DB. Short report: limited effectiveness of screening mammography in addition to clinical breast examination by trained nurse midwives in rural Jakarta, Indonesia. Int J Cancer. 2014;134(5):1250-1255.
- Okonkwo QL, Draisma G, der Kinderen A, Brown ML, de Koning HJ. Breast cancer screening policies in developing countries: a cost-effectiveness analysis for India. J Natl Cancer Inst. 2008;100(18):1290-1300.
- Mittra I, Mishra GA, Singh S, et al. A cluster randomized, controlled trial of breast and cervix cancer screening in Mumbai, India: methodology and interim results after three rounds of screening. Int J Cancer. 2010;126(4):976-984.
- Sankaranarayanan R, Ramadas K, Thara S, et al. Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst. 2011;103(19):1476-1480.
-
Buribekova R, Shukurbekova I, Ilnazarova S, et al. Promoting clinical breast evaluations in a lower middle-income country setting: an approach toward achieving a sustainable breast health program. J Glob Oncol. 2018;4:1-8.
-
Bhoo-Pathy N, Yip CH, Hartman M, et al. Breast cancer research in Asia: adopt or adapt Western knowledge? Eur J Cancer. 2013;49(3):703-709.
- Hassan LM, Mahmoud N, Miller AB, et al. Evaluation of effect of self-examination and physical examination on breast cancer. Breast. 2015;24(4):487-490.