Abstract
Mental health professionals’ moral intuitions about futility should prompt reevaluation of goals of care and care plans. Mostly, it will suffice to improve the care plan and/or slightly adjust the goal of care (eg, lower expectations), which is standard practice. Sometimes, however, all care plans that seek to reduce core symptoms (ie, that pursue a curative goal) are most likely futile and thus should not be imposed. Here, it may be in the patient’s best interest to change the goal of care toward palliation (ie, harm reduction, relief of suffering, and best possible quality of life). Thus, futility can function as a moral counterweight to the duty to treat, helping mental health professionals find the right balance between over- and undertreatment.
Moral Intuitions
– I wouldn’t want this for myself.
– Treatment is making my patient suffer horribly.
– There is no good option here.
– No matter what I do, I don’t think my patient is going to get better.
– I have no choice but to use coercion.
– I feel that we’re only making matters worse.
– I wouldn’t be surprised if my patient died this year.
Thoughts like these and associated feelings of unease, helplessness, and being stuck are not uncommon among mental health professionals, especially those caring for persons living with severe and persistent mental illness (SPMI).1,2 Typically, these concerns are dismissed or attributed to burnout, lack of training or experience, or unprofessional pessimism. Instead, this article explores these concerns as moral intuitions with the potential to improve care for persons living with SPMI.
Moral intuitions are thoughts that incline one toward a certain moral response (eg, We should not continue this patient’s current treatment) and arise without conscious effort. These inclinations are accompanied by a metacognitive feeling of (un)certainty: if all of the morally relevant information favors the same response, a sense of certainty drives the mental health professional to spontaneous action, often without their being aware of the underlying ethical dimension. If, however, the available information engenders competing responses (eg, to continue or curtail a burdensome treatment), an inclination may be accompanied or even eclipsed by a feeling of uncertainty. This is true of the moral intuitions and thoughts listed in the opening paragraph: the patient’s ill health and endangerment demand intervention, but, for some reason, this seems pointless or useless—in short, futile.
According to Cecchini,3 the resulting feeling of uncertainty about the appropriate moral response serves to prompt the mental health professional to engage in conscious reflection. However, while there is empirical evidence that mental health professionals make futility judgments in their clinical work,1,2,4 there are hardly any scientific contributions, practice recommendations, or tools to support reflection.5 As a first step toward bridging this gap, the present article offers some guidance for reflecting on instances of possible futility in mental health care.
Futility
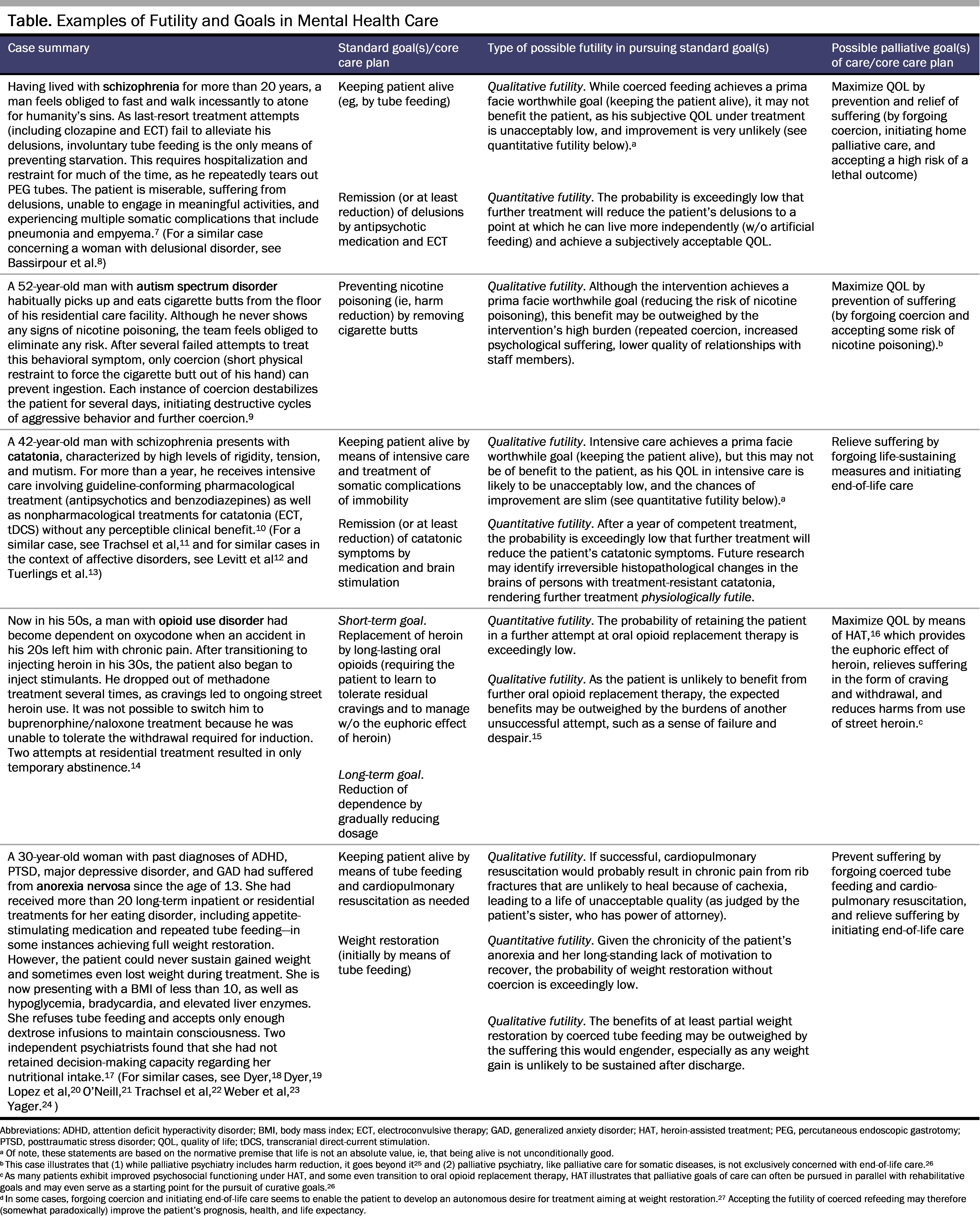
According to one common definition,6 physiological futility refers to instances in which a given treatment cannot possibly achieve the intended physiological effect. More often, in cases of quantitative futility, a treatment might have the intended effect, but the chances of success are unacceptably low. In cases of qualitative futility, a goal of care may be attainable with an acceptable level of probability, but attainment would fail to provide a significant benefit to the patient, or any treatment benefits would be outweighed by the associated burdens (for clinical examples, see the Table, columns 1-3).
Qualitative and quantitative futility share 3 ethically relevant characteristics: normativity, context independence, and specificity. First, futility is not simply an empirical issue but is inherently normative28—that is, it is based on values and not on facts alone (normativity). Judgments of quantitative futility require a cut-off value for the chance of success (between “low but just about acceptable” and “unacceptably low”), and this is itself a value-based decision. Qualitative futility is even more normatively driven because the benefit a person might derive from a given treatment is both highly personal and value based, as are the burdens that one may be willing to accept in pursuit of successful treatment. In the context of intensive care, the concept of futility has been heavily criticized for this normativity and discredited as a tool for paternalistic physicians to assert their own value-based judgments over patient wishes in withdrawing or withholding treatment.28 However, the mental health context is fundamentally different; in the most challenging situations, mental health professionals must decide whether to force treatment on an incompetent patient against their stated wishes or accede to their request to withdraw or withhold treatment. In many cases, patients have no valid advance directive29 and no close relationships, which means that there is no one to convey their autonomous wishes, preferences, and values.30 Here, substituted judgment is unfeasible, leaving mental health professionals (as well as judges, professional guardians, and others, depending on jurisdiction) with no choice but to make decisions according to the best interest standard.31 It follows that, in some cases, the duty to make value-based decisions for individuals with SPMI on the basis of minimal information about their autonomous wishes and personal values is inescapable.
Second, futility is independent of the macro context(eg, the respective health care system and jurisdiction) in the sense that it pertains to ideal circumstances (context independence). While pragmatic considerations (such as reimbursement schemes or laws on coercion) are important in devising good care plans, they are unrelated to futility. Care plans can be implementable and promising (eg, not futile), implementable but futile, promising but not implementable, and both futile and not implementable. Futility may allow for a nonmaleficence-based justification for withholding or withdrawing an intervention, from which follows the ethical obligation to offer or develop different interventions. Lack of implementability, perhaps due to lack of resources, may allow for a justice-based justification for withholding or withdrawing an intervention, from which follows the ethical obligation to develop just allocation schemes that ensure equitable access to health care. The importance of differentiating between futility and lack of implementability has been widely discussed in the context of ventilator allocation during the COVID-19 pandemic.32
Third, futility always pertains to a specific intervention, aiming at a specific goal of care, for a specific patient, at a specific moment in time.33,34 Of note, this specificity of futility is in stark contrast to mental health professionals’ often all-encompassing intuition about futility (eg, Nothing at all can be done anymore!). In addition, patient-related specificity includes, among other things, the ability of the patient to show the minimum cooperation required for the intervention to take effect.5 Care plans can become futile when mental health issues make it impossible for the patient to adhere to them (eg, when overwhelming fears of contamination prevent a patient from acting on her autonomous decision to take medication for her obsessive-compulsive disorder). Competent refusals of care plans, on the contrary, do not constitute cases of futility. The crucial difference is between not being able to cooperate with treatment and (autonomously) not wanting to do so.
Importantly, specificity opens up possibilities for coping with futility: to identify non-futile care plans, the original care plan can be improved and/or the goal of care can be changed. Other possible courses of action—turning to another patient or waiting for the chances of achieving the original goal of care to improve—could alleviate the professional’s futility-related distress but cannot answer the ethical question of how best to care for a given patient in the present moment. Therefore, those options are not pursued here.
Reflecting on Possible Futility
The flowchart in the Figure, which supports reflection on instances of possible futility, should ideally be used with colleagues, a supervisor, and/or a clinical ethicist. As goals in mental health care are often implicit, vague, or unclear, deliberation should start with clearly and explicitly formulating the current goal of care (step 1). The goal of care and the associated care plan should then be checked for futility (steps 2 and 3). If any of the questions cannot be answered affirmatively, pursuit of the current goal of care with the current care plan is likely currently futile for the patient in question and therefore inappropriate. In such cases, deliberation should focus on adjusting or changing the care plan (step 4) or the goal(s) of care (step 5). Given the high specificity of futility, such changes can help to sidestep the anticipated futility of the original goal of care or care plan.
While this flowchart was developed for reflection on care based on the best interest standard, it may also prove useful for preparing for shared decision making with competent patients or substitute decision makers. After elaborating different goals of care and associated care plans, the mental health professional should discuss all options with the patient or their substitute decision maker, clearly differentiating between professional knowledge and expertise (eg, estimated chances that a given care plan will achieve a given goal) and value judgments (eg, whether the burdens associated with a given care plan make this a chance worth taking). Finding alternative acceptable care plans with this flowchart may also be useful when the care plan that is deemed optimal by the mental health professional is (1) refused by a competent patient or substitute decision maker or (2) not implementable, keeping in mind that these scenarios do not constitute instances of futility and that they necessitate a different ethical justification for deviating from standards of care.
Figure. Flowchart for Reflection on Possible Futility in Mental Health Care
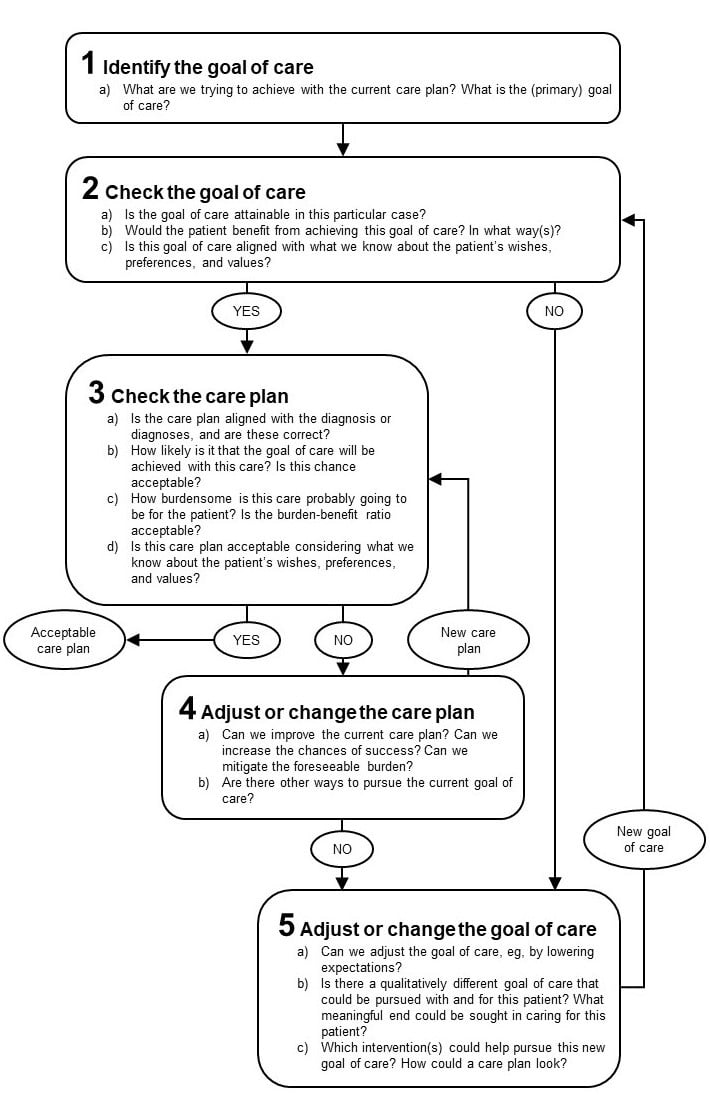
Reflection on possible futility can produce 1 of 3 broad outcomes: pseudo-futility, irrelevant futility, or futility of standard care.
Pseudo-futility. First, careful reflection may reveal that, contrary to a moral intuition or initial thought, the care plan is not futile for the case in question (all questions in steps 2 and 3 of the Figure are answered affirmatively). This pseudo-futility or subjective uncertainty about how best to care for the patient in question can originate from a lack of professional expertise or training (eg, regarding the probability or usual timing of a response to a specific intervention), the professional’s state of mind (eg, habitual pessimism, burnout), or the professional’s moral values (eg, who deserves treatment and which treatment is worthwhile). For example, procedures such as repeat heart surgery for endocarditis caused by intravenous drug use or removal of foreign bodies in the context of repetitive ingestion are sometimes refused on grounds of futility because there is a high risk of recidivism. However, the goal of care (to cure the endocarditis or remove the foreign object) is readily achieved, with benefits for the patient related to quality (and often also duration) of life. These scenarios may provoke debate about quality of care, resource allocation, and stigmatization, but they do not constitute instances of futility.35,36 However, even in cases of pseudo-futility, reflection on the possibility of futility is likely to prove more useful than outright rejection of the concept. In particular, guided reflection can improve mental health professionals’ awareness of their personal values and of the morally relevant features of clinical situations and increase their knowledge of relevant ethical concepts such as the fact-value distinction.37 These outcomes of reflection can mitigate the impact of intuitions surrounding instances of pseudo-futility on patient care. Future research should explore the “differential diagnosis” of futility to help mental health professionals identify instances of pseudo-futility more readily.
Irrelevant futility. Second, in cases of ethically irrelevant futility, professionals correctly conclude that (1) the care plan in question has an unacceptably low chance of achieving its goals or entails an unacceptably low benefit-burden ratio, rendering the care plan futile. However, (2) this shortcoming is easily rectified by optimizing the care plan (eg, switching the antipsychotic medication to clozapine; step 4 in the Figure) or slightly adjusting the goal of care (eg, lowering weight gain expectations from a pound to a half pound per week; step 5a in the Figure). The clinical literature is replete with tips, strategies, and recommendations of this kind, often associated with keywords like “nonresponder” or “treatment-resistant.” A glaring example of ethically irrelevant futility is treatment based on wrong diagnoses (eg, monotherapy with antipsychotics for auditory flashbacks in borderline personality disorder misdiagnosed as demeaning voices in schizophrenia). While it may pose a clinical challenge to correctly diagnose a specific patient, this scenario does not pose an ethical challenge, as there is an unambiguously better care plan within standard care. Whether or not we categorize such instances as futility as opposed to suboptimal, incompetent, or inappropriate care is irrelevant from an ethical point of view, as optimizing the care plan is ethically mandated in any case. Nevertheless, explicit reflection on instances of (ethically) irrelevant futility is (clinically) relevant, as it can improve patient care and provide learning opportunities for mental health professionals.
Futility of standard care. Third, questions of futility become ethically relevant when they concern all standard care plans or standard goals of care for a given patient (futility of standard care; for examples, see Table, columns 2-3). Needless to say, mental health professionals should exert extreme caution here. Until guidelines on this issue are published, we suggest consulting at least 2 independent experts on the patient’s condition. Should their advice yield an acceptable care plan, the matter would be identified as pseudo- or irrelevant futility. Otherwise, it may be reasonable to conclude that there is no care plan that would offer an acceptable chance of success and benefit-burden ratio, even for a scaled-down version of the original goal of care. To address the ensuing ethical challenge of being obligated to provide care in the face of probable futility of standard care, we propose a qualitative shift in the goal(s) of care (see the Figure, steps 5b and 5c).
Goals of Mental Health Care
By default, the goals of mental health care are curative in the sense that they focus on the alleviation of core symptoms of mental disorders—that is, diagnostic criteria such as delusions, catatonic symptoms, inability to control substance use, and restrictive eating (see Table, column 2).15,38 Although mental health care often addresses symptoms rather than causes and achieves only partial symptom reduction rather than complete remission, as long as the focus is on reducing core symptoms, the goals of care remain curative.38 Qualitatively different are rehabilitative and palliative goals of care. The overarching rehabilitative goal in mental health care is to improve the psychosocial functioning of persons living with SPMI—in other words, the development of “the emotional, social and intellectual skills needed to live, learn and work in the community with the least amount of professional support.”39 This means, for example, that “symptom control does not necessarily have the highest priority, as some side effects of pharmacological treatment can weaken a person’s ability to perform his or her social roles, and impair vocational rehabilitation.”39
Given that, in some cases, even the pursuit of rehabilitative goals of care is likely futile, some have advocated the implementation of palliative approaches to mental health care (ie, palliative psychiatry).15,26,40,41 The overarching palliative goal in mental health care is to maximize quality of life through harm reduction and relief of suffering.26 While curative psychiatry also seeks to improve quality of life, these approaches differ in 2 respects. First, in terms of strategies applied, curative psychiatry strives to improve quality of life through reduction of core symptoms, while palliative psychiatry aims to reduce harms and relieve suffering by working around core symptoms of the SPMI.26 For example, anorexia nervosa often reduces quality of life because underweight-related fatigue limits the social activities the patient can partake in. A curative approach would aim at increasing weight and thus tackle a core symptom of anorexia nervosa, which—if successful—is likely to indirectly enable the patient to be more active, thereby improving her quality of life. A palliative approach would directly aim at improving quality of life by, for example, arranging weekly home visits by an experienced mental health nurse to alleviate loneliness without pushing for weight gain. The second difference relates to time frames: while curative psychiatry seeks to improve the patient’s future quality of life—sometimes accepting an undesired but foreseen reduction of current quality of life by side effects or coercive measures—palliative psychiatry prioritizes current quality of life. For example, abstinence-oriented treatment for opioid use disorder prioritizes the hope of a better quality of life after successful treatment over current quality of life, which is reduced by withdrawal and craving, while heroin-assisted treatment prioritizes current quality of life, which is improved by relief of craving and induction of euphoria (see Table, line 5 for a clinical example).
While palliative goals of care often can (and should) be integrated with rehabilitative and curative goals,26 sometimes mental health professionals must prioritize one goal over the others (eg, when having to decide whether to impose burdensome treatment of doubtful effectiveness in the face of acute endangerment of a patient whose autonomous wishes and values are unknown). In such challenging situations, futility can act as a moral counterweight to the duty to treat, helping mental health professionals find the right balance between over- and undertreatment. In instances of futility of curative and rehabilitative care plans, the palliative goal of preventing suffering may justifiably be prioritized over any other goal, sometimes even over the minimal goal of keeping the patient alive.
In conclusion, futility of standard care calls for not imposing the care plan(s) in question, but it does not relieve mental health professionals of the general obligation to provide care. To fulfill this obligation of providing care in the face of futility of standard care, mental health care as a discipline needs to develop, evaluate, and provide alternative approaches to standard care, such as palliative psychiatry.
References
- Brodwin P. Futility in the practice of community psychiatry. Med Anthropol Q. 2011;25(2):189-208.
-
Stoll J, Mathew A, Venkateswaran C, Prabhakaran A, Westermair AL, Trachsel M. Palliative care for patients with severe and persistent mental illness: a survey study of the attitudes of psychiatrists in India compared to psychiatrists in Switzerland. Front Psychiatry. 2022;13:858699.
- Cecchini D. Dual-process reflective equilibrium: rethinking the interplay between intuition and reflection in moral reasoning. Philos Explor. 2021;24(3):295-311.
-
Trachsel M, Hodel MA, Irwin SA, Hoff P, Biller-Andorno N, Riese F. Acceptability of palliative care approaches for patients with severe and persistent mental illness: a survey of psychiatrists in Switzerland. BMC Psychiatry. 2019;19:111.
-
Levitt S, Buchman DZ. Applying futility in psychiatry: a concept whose time has come. J Med Ethics. 2020;47(12):e60.
-
Pope TM. Medical futility. In: Hester DM, Schonfeld T, eds. Guidance for Healthcare Ethics Committees. Cambridge University Press; 2012:88-97.
- Rosenbaum DMS, Robertson D, Law S. Psychiatric futility and palliative care for a patient with clozapine-resistant schizophrenia. J Psychiatr Pract. 2022;28(4):344-348.
- Bassirpour G, Mahr G, Lee B, Torres M. The use of hospice care in end-stage psychiatric patients. J Palliat Med. 2011;14(1):107-108.
-
Decorte I, Verfaillie F, Moureau L, et al. Oyster care: an innovative palliative approach towards SPMI patients. Front Psychiatry. 2020;11:509.
- Baldinger-Melich P, Fugger G, Kraus C, et al. Treatment-resistant catatonia—a case report. Clin Neuropsychiatry. 2016;13(2):24-27.
-
Trachsel M, Johnsen C, Elgudin J. Palliative psychiatry: a new field for treatment-resistant mental illness. Paper presented at: Annual Meeting of the American Psychiatric Association; May 20-24, 2022; New Orleans, LA.
- Levitt G. Serious mental illness and hospice care. J Palliat Care. 2022;37(1):13-14.
- Tuerlings JHAM, Müller METM, Verwey B, van Waarde JA. Palliative care in a psychiatric-somatic care unit. Article in Dutch. Ned Tijdschr Geneeskd. 2008;152(36):1949-1952.
- Jun JH, Fairbairn N. Integrating injectable opioid agonist treatment into a drug treatment court program: a case study. Subst Abus. 2018;39(4):493-496.
- Berk M, Berk L, Udina M, et al. Palliative models of care for later stages of mental disorder: maximizing recovery, maintaining hope, and building morale. Aust N Z J Psychiatry. 2012;46(2):92-99.
- Strang J, Groshkova T, Uchtenhagen A, et al. Heroin on trial: systematic review and meta-analysis of randomized trials of diamorphine-prescribing as treatment for refractory heroin addiction. Br J Psychiatry. 2015;207(1):5-14.
- Sawhill C, Fipps DC, Palomo JV, Miller M. End-stage anorexia nervosa: when to say “when.” A literature review of an ethically complicated case. Psychosomatics. 2020;61(6):779-786.
-
Dyer C. Anorexic woman cannot be force fed, judge rules. BMJ. 2012;345:e5804.
-
Dyer C. Anorexia patient should not be subject to any more compulsory treatment, court rules. BMJ. 2014;349:g6184.
- Lopez A, Yager J, Feinstein RE. Medical futility and psychiatry: palliative care and hospice care as a last resort in the treatment of refractory anorexia nervosa. Int J Eat Disord. 2010;43(4):372-377.
- O’Neill J, Crowther T, Sampson G. A case study: anorexia nervosa. Palliative care of terminal psychiatric disease. Am J Hosp Palliat Care. 1994;11(6):36-38.
- Trachsel M, Wild V, Biller-Andorno N, Krones T. Compulsory treatment in chronic anorexia nervosa by all means? Searching for a middle ground between a curative and a palliative approach. Am J Bioeth. 2015;15(7):55-56.
-
Weber S, Paulzen M, Elsner F, et al. Wegen anorexia nervosa auf die palliativstation? Does anorexia nervosa qualify for specialized palliative care? Nervenarzt. 2023;94(7):631-633.
-
Yager J. Managing patients with severe and enduring anorexia nervosa: when is enough, enough? J Nerv Ment Dis. 2020;208(4):277-282.
- Westermair AL, Buchman DZ, Levitt S, Trachsel M. Palliative psychiatry for severe and enduring anorexia nervosa includes but goes beyond harm reduction. Am J Bioeth. 2021;21(7):60-62.
- Westermair AL, Buchman DZ, Levitt S, Perrar KM, Trachsel M. Palliative psychiatry in a narrow and in a broad sense: a concept clarification. Aust N Z J Psychiatry. 2022;56(12):1535-1541.
-
Mishra R. What actually happened. Camb Q Healthc Ethics. 2012;21(3):408.
-
White D, Pope T. Medical futility and potentially inappropriate treatment. In: Youngner SJ, Arnold RM, eds. The Oxford Handbook of Ethics at the End of Life. Oxford University Press; 2016:65-86.
- Pope TM. Making medical decisions for patients without surrogates. N Engl J Med. 2013;369(21):1976-1978.
- Friesen P, Gligorov N. Surrogate decision making for unrepresented patients: proposing a harm reduction interpretation of the best interest standard. Clin Ethics. 2020;15(2):57-64.
-
Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 8th ed. Oxford University Press; 2019.
- Truog RD, Mitchell C, Daley GQ. The toughest triage—allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973-1975.
- Mohindra RK. Medical futility: a conceptual model. J Med Ethics. 2007;33(2):71-75.
- Coulter A, Schuermeyer I, Sola C. Evaluating ineffective treatments: a proposed model for discussing futility in psychiatric illness. Harv Rev Psychiatry. 2021;29(3):240-245.
- Goldberg A. A futile use of futility. Hastings Cent Rep. 2020;50(4):4-5.
- Lytle S, Stagno SJ, Daly B. Repetitive foreign body ingestion: ethical considerations. J Clin Ethics. 2013;24(2):91-97.
-
McMillan J. The Methods of Bioethics: An Essay in Meta-Bioethics. Oxford University Press; 2018.
- Goldberg JF. When further pharmacotherapy seems futile. J Clin Psychiatry. 2018;80(1):1-2.
- Rössler W. Psychiatric rehabilitation today: an overview. World Psychiatry. 2006;5(3):151-157.
-
Trachsel M, Irwin SA, Biller-Andorno N, Hoff P, Riese F. Palliative psychiatry for severe persistent mental illness as a new approach to psychiatry? Definition, scope, benefits, and risks. BMC Psychiatry. 2016;16:260.
-
Strand M, Sjöstrand M, Lindblad A. A palliative care approach in psychiatry: clinical implications. BMC Med Ethics. 2020;21:29.