Abstract
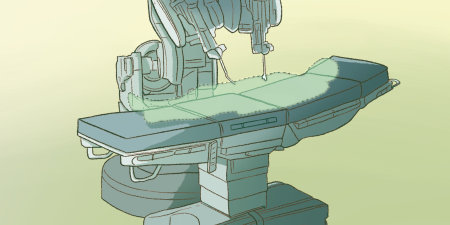
The surgical platform for robotic-assisted surgery has enabled many surgeons to join a popular trend in minimally invasive surgery, which offers prospective benefits to patients (eg, shorter hospital stays, earlier recovery, and less pain) and operational benefits to surgeons. Surgeons without minimally invasive surgical training typically acquired during fellowship training are generally able to perform complex procedures with the robotic platform due to its ergonomic suturing instrumentation, tremor stabilization, 3D visualization, and 4-arm control by a single surgeon. Prospective benefits, however, must be balanced against prospective risks. This article explores the multitude of factors that persuade both surgeons and patients to choose robotic surgery over open surgery or conventional laparoscopy and explores whether evidence exists to support its use despite sometimes conflicting research.
History of Minimally Invasive Surgery
Minimally invasive surgery (MIS) has come a long way in the more than 120 years since gynecologist Dimitri Ott examined the peritoneal cavity of a woman in 1901 with a head mirror and a speculum through a culdoscopic opening.1,2 Almost 85 years later, in 1985, Erich Mühe performed the first laparoscopic cholecystectomy in Germany.2,3 The change to the surgical field that laparoscopy brought about has been one of the most revolutionary in the history of surgery. Prior to the 1990s, the surgical dogma was “the bigger the cut, the better the surgeon.” This attitude began to change with the shift to not only less invasive surgery but also surgical practices that were driven by popular patient demand.4 It was estimated that, by 1992, about 80% of cholecystectomies were being performed laparoscopically,5 and laparoscopic cholecystectomy has since become the gold standard of care for patients worldwide suffering from biliary colic. The explosion of interest in this novel technique was driven by patient demand for surgeries whose incisions could be covered with mere band-aids at the completion of the case. Patients wanted smaller scars, less pain, and less recovery time.
A further evolution of MIS came through the development of remote robotic telesurgery for use in battlefields and since adopted for use in many surgical specialties.6 Over the years, this advancement has been proven to produce—at the very least— technical outcomes not inferior to those afforded by comparable laparoscopic procedures and, in some cases, superior to them.7,8,9,10 This paper explores the factors that persuade both surgeons and patients to favor robotic surgery over laparoscopic surgery as well as the possible reasons that conflicting research exists to support its use.
Enhanced Operative Experience
Surgeons’ operative experience differs considerably with the robotic platform. Improved ergonomics by enabling surgeons to sit at a customizable console—and to operate with increased dexterity, tremor reduction, 3D visualization, up to 10 times magnification, and control of 4 arms—are all ways that simplify MIS for those not trained to operate laparoscopically.11,12 Consequently, surgeons who have not embraced laparoscopic procedures routinely in their practice can now make the transition to MIS with relative ease through the robotic platform. While rigid laparoscopic instruments provide 4 degrees of motion, robotic instruments have 7, mimicking the human wrist through EndoWrist technology.11 By increasing dexterity in ways that laparoscopic techniques cannot accommodate, robotic operating makes suturing easier for those who have limited or no training in MIS.13
Despite the benefits of robotic surgery for surgeons, evidence that the shift to robotic surgery is due primarily to a decline in open surgery is not robust. One review article did conclude that robotic lobectomies are increasing while open lobectomies are decreasing and lobectomies performed by video-assisted thoracoscopic surgery (a laparoscopic equivalent) are remaining stable.14 Similarly, a cohort study that included over 169 000 patients from 73 Michigan hospitals found that while the use of robotic surgery overall increased from 1.8% of cases in 2012 to 15.5% of cases in 2018—and 41-fold over the same time period for certain procedures, such as inguinal hernia repair—use of laparoscopy, which had increased by 1.3% per year prior to the adoption of robotics, afterwards declined by 0.3% per year.15 While these findings suggest that surgeons who use open surgery are transitioning to robotic surgery, a 7-year retrospective review published in 2018 found that while use of robotic surgeries increased in all 5 categories (colectomies, cholecystectomies, bariatric surgeries, inguinal and ventral hernia repairs), use of laparoscopic procedures decreased relative to use of robotic procedures, leading the authors to conclude that the increase in robotic surgeries came from laparoscopic surgeons utilizing more robotics rather than from open surgeons converting to robotic surgery.16 This conclusion, however, is limited by the fact that new surgeons entering the surgical field were not accounted for, and individual surgeon case data were not available. The data also showed that the highest absolute increase in use of robotics was for colectomies and bariatric surgeries (from 0.1% to 3.1% and from 0.4% to 4.8%, respectively), which surgeries also had the highest absolute decrease in open procedures (from 71.8% to 61.9% and from 20.1% to 10.1%, respectively), raising the question of whether the increased use of robotic surgery for these procedures comes from a technical advantage due to the greater complexity of those cases. All in all, it is difficult to generalize these trends accurately without looking at individual surgeons’ data and accounting for new trainees entering the field.
Making Procedures Safer, Faster, Cheaper
Critics frequently cite the longer operating times and higher costs of robotic surgery compared to laparoscopic surgery,9,10,11 but history provides a more nuanced perspective. The first laparoscopic cholecystectomy took 2 hours to complete.1 Now experienced surgeons can perform that same procedure in under 30 minutes.17 Similarly, studies conducted in the 1990s comparing laparoscopic to open appendectomies showed that laparoscopic procedures cost the hospital more money and took longer to complete as well.1 Now open appendectomies generally occur only in unusual circumstances, and one would be hard-pressed to find a patient who would choose an open appendectomy over a laparoscopic one. Residents trained today are more comfortable and more experienced with laparoscopic appendectomies and laparoscopic cholecystectomies than the same procedures done open. As surgeons become more experienced using the robot, they are able to use fewer instruments in more versatile ways, resulting in decreased instrument exchanges, all contributing to decreased cost and operating room time.18
Robotic Platforms in Education
Surgical residents have a minimum requirement to complete 100 basic laparoscopic cases in addition to 75 complex laparoscopic cases in order to fulfill graduation requirements.19 Recently, an option to log cases as robotic has become available for general surgery and obstetrics-gynecology residents, and urology residents have an already-established 80 case minimum requirement for robotic procedures.20 It seems that it is only a matter of time before robotic training becomes a standardized, integral part of basic training for all surgeons. As the robotic platform continues to be utilized and as the instruments and technology continue to evolve, surgeons will continue to reduce not only operative time, but also cost per procedure, making it possible to believe that, with improved training, the cost and time difference between laparoscopic and robotic surgery will be negligible.16 Currently, robotic training consists of web-based and dedicated on-site training programs, virtual reality skills simulation, and old-fashioned mentorship that residents are exposed to during their training.21 These opportunities, however, are not standardized within residency programs across the United States, and access to them is widely variable.
An equilibrium needs to be achieved between enthusiasm for advancements and a healthy dose of skepticism to ensure safety of novel procedures due to initial uncertainty.
Intuitive Surgical, Inc, the company behind the da Vinci robotic platform—currently the most widely used platform in the United States22—has training simulations available online and on the operating console, allowing trainees to practice transferable skills outside of the operating room, without compromising patient safety.21 The company also has a system in place for experienced robotic surgeons to proctor surgeons new to robotic surgery, now also available via an easy-to-use platform, the Intuitive Hub, which allows for video recording and virtual collaboration in real time and after the procedure is complete by enabling surgeons to review and track progress. This unique learning platform allows surgeons in all stages of training to broaden their robotic skills and adapt robotics to their practice faster than before. The app collects data during operations by tracking the surgeon’s every move, instrument changes, clutch use, and so on and provides feedback in order to assess and improve efficiency and to compare the surgeon’s personal results to those of other surgeons. This technology will also help address access issues and can allow residency programs to establish set goals for residents to achieve throughout their training.
Outcomes for Surgeons
Complex cases may offer a greater advantage when done robotically than laparoscopically for surgeons with less training in MIS. In a systematic review, Flynn et al found that operating times for robotic colectomies were shorter than for laparoscopic colectomies when the surgeons were unfamiliar with both platforms.23 Although Lauka et al’s systematic review and meta-analysis found that operative times were longer and costs higher for robotic right colectomies than for laparoscopic right colectomies, 3 of the studies included took into account the effect of experience on operative time and showed that operative times decreased for robotic colectomies over the course of the learning curve,24,25,26 and 1 of the 3 studies further reported that, for 11 to 20 completed cases, robotic right hemicolectomies took less time to complete than laparoscopic, likely due to a shorter learning curve.25 Moreover, robotic colectomies had lower conversion rates, less estimated blood loss, higher lymph node harvest, and a shorter hospital stay than laparoscopic colectomies.10
In light of these findings, the results discussed earlier favoring open or laparoscopic procedures over robotic procedures may be due to the operative background of the surgeons participating in the studies, as hypothesized by Edward Felix.27 Surgeons who have a diverse laparoscopic background and who are highly proficient in laparoscopy might have increased frustration as well as longer operative times with equivalent robotic cases simply due to being less familiar with the platform despite its advantages. This hypothesis may explain why the results of similar studies reach variable conclusions.
Patient Preference and Robotic Surgery
Minimally invasive procedures have been shown to be not only better for patients in terms of reduced recovery time and pain but also the method preferred by patients, resulting in greater satisfaction.15,28 Less time in the recovery unit after the procedure, as well as decreased narcotic use due to less postoperative pain after hernia repair, has considerable implications for both the patient and the health system.29 An evidence-based analysis published by the Medical Advisory Secretariat of Health Quality Ontario found that, compared to laparoscopic hysterectomies, robotic hysterectomies had fewer conversions to open surgery (which had significantly greater blood loss and longer hospitalization time than either minimally invasive modality), resulting in reduced morbidity.30 The same analysis found that robotic prostatectomies for prostate cancer had a significant decrease in blood loss and therefore fewer transfusions, had a decreased incidence of positive surgical margins, and had decreased erectile dysfunction compared to laparoscopic prostatectomies.31
During the development of laparoscopy, however, randomized controlled trials were challenging to conduct due to attrition bias32; studying various techniques in surgery depends on patients’ cooperation. As technology advances and becomes more futuristic, patients want the new and the popular, even if it may not necessarily be supported by scientific evidence. Surgeons must be cognizant of this fact and remember the many historical instances in which great discoveries in the medical field were greeted with disparagement and a considerable lag time to acceptance in the medical community (think Louis Pasteur’s germ theory and Semmelweis’ theory of the cause of puerperal fever). Similarly, laparoscopic gallbladder operations were deemed dangerous and unethical during the early days of their use.33 An equilibrium needs to be achieved between enthusiasm for advancements and a healthy dose of skepticism to ensure safety of novel procedures due to initial uncertainty. All of this is to say that, despite the aforementioned barriers, continued high-quality investigations still need to be done to fully understand the rapidly evolving impact that robotic surgery has on patients, surgeons, and society.
Behind the Knife, a popular podcast among surgeons and surgical trainees alike, has interviewed nationally and world-renowned surgeons, such as John Cameron and Carlos Pellegrini. When asked what has been the single greatest innovation in surgery over the course of their careers, overwhelmingly the answers have included MIS.34 Above all, in light of ever-increasing and dynamic evidence, it is important for patients and surgeons to work together to understand the differences in techniques and their uses and applications, to dissipate misunderstandings, and to come up with a final best option of treatment in each case.
References
- Himal HS. Minimally invasive (laparoscopic) surgery. Surg Endosc. 2002;16(12):1647-1652.
- Polychronidis A, Laftsidis P, Bounovas A, Simopoulos C. Twenty years of laparoscopic cholecystectomy: Philippe Mouret—March 17, 1987. JSLS. 2008;12(1):109-111.
- Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS. 2001;5(1):89-94.
- Schlich T, Tang CL. Patient choice and the history of minimally invasive surgery. Lancet. 2016;388(10052):1369-1370.
-
National Institutes of Health Consensus Development Conference Statement on Gallstones and Laparoscopic Cholecystectomy. Am J Surg. 1993;165(4):390-398.
-
George EI, Brand TC, LaPorta A, Marescaux J, Satava RM. Origins of robotic surgery: from skepticism to standard of care. JSLS. 2018;22(4):e2018.00039.
- Qabbani A, Aboumarzouk OM, ElBakry T, Al-Ansari A, Elakkad MS. Robotic inguinal hernia repair: systematic review and meta-analysis. ANZ J Surg. 2021;91(11):2277-2287.
- Gerdes S, Burger R, Liesch G, et al. Results of robotic TAPP and conventional laparoscopic TAPP in an outpatient setting: a cohort study in Switzerland. Langenbecks Arch Surg. 2022;407(6):2563-2567.
- Aiolfi A, Cavalli M, Micheletto G, et al. Robotic inguinal hernia repair: is technology taking over? Systematic review and meta-analysis. Hernia. 2019;23(3):509-519.
-
Lauka L, Brunetti F, Beghdadi N, Notarnicola M, Sommacale D, de’Angelis N. Advantages of robotic right colectomy over laparoscopic right colectomy beyond the learning curve: a systematic review and meta-analysis. Ann Laparosc Endosc Surg. 2020;5:33.
- Anderson PL, Lathrop RA, Herrell SD, Webster RJ 3rd. Comparing a mechanical analogue with the Da Vinci user interface: suturing at challenging angles. IEEE Robot Autom Lett. 2016;1(2):1060-1065.
- Valdivieso RF, Zorn KC. Practice makes progress: assessing our robotic skills. Can Urol Assoc J. 2013;7(11-12):435-436.
- Palep JH. Robotic assisted minimally invasive surgery. J Minim Access Surg. 2009;5(1):1-7.
-
Louie BE, Vallieres E. Transitioning from open to robotic lung surgery. Video-assist Thorac Surg. 2020;5:26.
-
Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. 2020;3(1):e1918911.
- Armijo PR, Pagkratis S, Boilesen E, Tanner T, Oleynikov D. Growth in robotic-assisted procedures is from conversion of laparoscopic procedures and not from open surgeons’ conversion: a study of trends and costs. Surg Endosc. 2018;32(4):2106-2113.
- Jackson TD, Wannares JJ, Lancaster RT, Rattner DW, Hutter MM. Does speed matter? The impact of operative time on outcome in laparoscopic surgery. Surg Endosc. 2011;25(7):2288-2295.
-
Feldstein J, Coussons H. Achieving robotic program best practice performance and cost versus laparoscopy: two case studies define a framework for optimization. Int J Med Robot. 2020;16(3):e2098.
-
Accreditation Council for Graduate Medical Education. Defined category minimum numbers for general surgery residents and credit role. Accreditation Council for Graduate Medical Education; 2019. Accessed January 22, 2023. https://www.acgme.org/globalassets/definedcategoryminimumnumbersforgeneralsurgeryresidentsandcreditrole.pdf
-
Accreditation Council for Graduate Medical Education. Case log information: urology. Accreditation Council for Graduate Medical Education; 2022. Accessed January 22, 2023. https://www.acgme.org/globalassets/pfassets/programresources/480-urology-case-log-info.pdf
-
Chen R, Rodrigues Armijo P, Krause C, Siu KC, Oleynikov D; SAGES Robotic Task Force. A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc. 2020;34(1):361-367.
-
Top 8 robotic surgery companies in the United States. IData Research. August 8, 2022. Accessed May 2, 2023. https://idataresearch.com/top-robotic-surgery-companies-in-the-united-states/
- Flynn J, Larach JT, Kong JCH, Waters PS, Warrier SK, Heriot A. The learning curve in robotic colorectal surgery compared with laparoscopic colorectal surgery: a systematic review. Colorectal Dis. 2021;23(11):2806-2820.
- Spinoglio G, Bianchi PP, Marano A, et al. Robotic versus laparoscopic right colectomy with complete mesocolic excision for the treatment of colon cancer: perioperative outcomes and 5-year survival in a consecutive series of 202 patients. Ann Surg Oncol. 2018;25(12):3580-3586.
- de’Angelis N, Lizzi V, Azoulay D, Brunetti F. Robotic versus laparoscopic right colectomy for colon cancer: analysis of the initial simultaneous learning curve of a surgical fellow. J Laparoendosc Adv Surg Tech A. 2016;26(11):882-892.
- Mégevand JL, Amboldi M, Lillo E, et al. Right colectomy: consecutive 100 patients treated with laparoscopic and robotic technique for malignancy. Cumulative experience in a single centre. Updates Surg. 2019;71(1):151-156.
-
Felix EL. Robotic surgery: “deja vu all over again.” General Surgery News. March 9, 2021. Accessed September 28, 2022. https://www.generalsurgerynews.com/Opinion/Article/03-21/Robotic-Surgery-D-j-agrave-Vu-All-Over-Again-/62765
- Shyr BU, Shyr BS, Chen SC, Chang IW, Shyr YM, Wang SE. Operative results and patient satisfaction after robotic pancreaticoduodenectomy. Asian J Surg. 2020;43(4):519-525.
-
McCoy K, Symons W, Clarke J, Novack M, Broderick M. Open versus robotic inguinal hernia repair: is there a superior approach? Poster presented at: SAGES Annual Meeting; March 22-25, 2017; Houston, TX. Accessed November 4, 2022. https://www.sages.org/meetings/annual-meeting/abstracts-archive/open-versus-robotic-inguinal-hernia-repair-is-there-a-superior-approach/
- Medical Advisory Secretariat. Robotic-assisted minimally invasive surgery for gynecologic and urologic oncology: an evidence-based analysis. Ont Health Technol Assess Ser. 2010;10(27):1-118.
-
Du Y, Long Q, Guan B, et al. Robot-assisted radical prostatectomy is more beneficial for prostate cancer patients: a system review and meta-analysis. Med Sci Monit. 2018;24:272-287.
-
Jaschinski T, Mosch CG, Eikermann M, Neugebauer EAM, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11(11):CD001546.
- Litynski GS. Erich Mühe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS. 1998;2(4):341-346.
-
Bingham J, Kniery K, Steele S. #4: John Cameron, MD Johns Hopkins, pancreas cancer and the Whipple. Behind the Knife. April 14, 2015. Accessed September 20, 2022. https://behindtheknife.org/podcast/4-john-cameron-m-d-johns-hopkins-pancreas-cancer-and-the-whipple/