Case
Jenny is a third-year medical student on her internal medicine rotation at the Veterans Administration Hospital. The rotation has been a great learning experience; her patients are generally friendly and grateful for the care they are receiving.
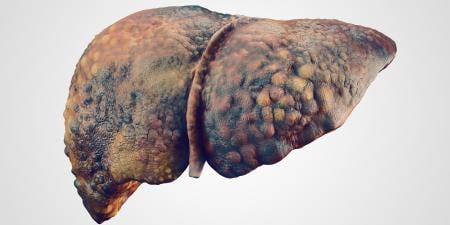
One of Jenny's favorite patients is Mr. Hackman, a 53-year-old veteran who has been diagnosed with alcoholic cirrhosis and is currently on the transplant waiting list. Every afternoon Jenny talks with Mr. Hackman, and he often shares stories with her about the past. Jenny takes a genuine interest in the stories about his family and supports his attempts at sobriety. During one of their sessions, Mr. Hackman revealed that he had taken a drink at a friend's house 2 months prior. He swore that this was "the only drink I've had in the last 2 years." He pleaded with Jenny not to tell anyone about his transgression because he knew that alcohol abuse could affect his status on the transplant list.
Commentary 3
To tell or not to tell? That is the dilemma facing Jenny as a member of the team caring for Mr. Hackman. Clearly, Jenny has an emotional attachment to Mr. Hackman, and this is very common in clinical medicine. But when clinical decisions potentially impact the care of other patients, objectivity must guide the physician's decision.
As you, Jenny, approach this case, you must clarify several issues before deciding what to do. First, what are the medical facts and allocation policies regarding liver transplantation in patients with alcoholic liver disease? What are the survival figures for patients with alcoholic liver disease who receive new livers? What is the rate of alcohol recidivism for transplant recipients like Mr. Hackman? Does the admission of alcohol use permanently eliminate Mr. Hackman from consideration for a transplant? Will he get a second chance if he is removed from his current spot on the list? What are the implications for other patients on the waiting list if Mr. Hackman remains on the list and receives a transplant? Should you withhold this information and "protect" Mr. Hackman's chance of getting a transplant? Careful examination of these questions will lead you toward a thoughtful and informed decision.
In the early days of liver transplantation, alcoholic liver disease was the most frequent indicator for liver transplants. Hepatitis C has now become the major indication, but many hepatitis C patients also have histories of alcohol dependence. Survival figures for patients with alcoholic liver disease who have received transplants have been excellent, comparable to the success rates among those who received liver transplants because of non-alcohol-related reasons. In fact, survival rates after transplant for patients with alcoholic liver disease are better than those for patients who received livers because of chronic hepatitis C alone. The major concern in transplant patients with alcoholic liver disease is recidivism—how many patients return to drinking following the transplant. Dr. Thomas Starzl, the "father" of liver transplantation in the United States, proposed that a liver transplant was the "ultimate 'sobering' experience."1 This comment suggests that patients with alcoholic liver disease do not drink following a transplant. Unfortunately, this has not been proven true. Recognizing this, transplant centers now require a period of abstinence before a transplant. This period of abstinence demonstrates 2 important things to the transplant team. First, alcohol abstinence remains the most effective treatment for alcoholic hepatitis, so many patients improve during the period of abstinence and, as a result, their need for a transplant is not as urgent. Second, the period of abstinence shows some degree of commitment by the patient. The longer the pretransplant abstinence lasts, the greater the chance of long-term abstinence. At least 5 years of sobriety is necessary before a reasonable chance of long-term abstinence is present.2 Due to the severity and complications of their disease, many patients do not have that much time. Yet many centers require at least a 6-month period of sobriety, often with random drug and alcohol screens, before a patient is placed on the waiting list.
Liver transplantation, in general, is plagued by the recurrence of the original disease in the liver allograft. Hepatitis C is the best example of this because Hepatitis C viremia is not eliminated at the time of the transplant, making infection of the allograft inevitable. The cause of recurrence is different in alcoholic liver disease where the disease reappears only if the transplant recipient relapses to alcohol dependence. Multi-centered studies have examined the experience of disease recurrence,3,4,5,6 many using patient interviews and recall, eg, "Have you had alcohol since your transplant?" Obviously, this method is dependent on patient recollection and honesty. The studies found that the prevalence of alcohol ingestion increased with the length of time since the transplant, with the rate of recidivism reaching 50 percent after 5 years in some series.3,4 Fortunately, the incidence of "problem" drinking, ie, drinking to the point of medical complications, was relatively rare, affecting only 10 percent of patients.6 Thus, there may actually be some truth to the "ultimate sobering experience" observation by Dr. Starzl years ago.
Another potential consideration in Jenny's decision is the severity of Mr. Hackman's illness. Deceased donor liver allocation is currently based on the severity of the would-be recipient's illness. The model for end-stage liver disease (MELD) uses 3 easily obtainable lab values (serum bilirubin, serum creatinine, and INR) to generate a "score" as a means of predicting a 3-month mortality risk. The higher the MELD score, the higher the risk of death, and the higher the patient's place on the transplant list. Therefore, if Mr. Hackman's MELD score is high, he may be "too sick" to survive any additional time on the waiting list. Many centers tell patients that the 6 month "clock" starts over after each use of alcohol, meaning they must remain abstinent another full 6 months before returning to the waiting list. If Mr. Hackman has a predicted 80 percent risk mortality in the next 3 months, waiting to get back on the transplant list may not be an option, and Jenny may think she is giving him a death sentence if she reports his "slip" into alcohol consumption. If his MELD score is relatively low, however, coming off the list could allow Mr. Hackman to seek additional counseling or treatment that could ultimately lead to a prolonged period of abstinence, both before and after the transplant. Jenny's decision to tell the transplant team might ultimately be better for Mr. Hackman if his state of health permits him to survive the consequence.
Jenny must also consider the potential effect of her decision on other patients. Mr. Hackman is 1 of over 18 000 patients on the nationwide liver transplant waiting list. If he gets the transplant, someone else does not. This reality often prompts people to ask "whose life is worth more?" This is not how transplant teams make decisions regarding the waiting list. Rather, the question that the transplant team must answer is "does any single patient have an acceptable risk of mortality and an acceptable potential for posttransplant survival?" Alcohol recidivism is only 1 of many factors taken into account. Medical comorbidities, previous surgeries, and psychosocial support are equally important and carefully considered.
Finally, Jenny must carefully consider her own emotional attachment to Mr. Hackman and his family and take an objective look at her feelings. How long has she known him? Did she just meet him a few days ago at the time of a hospital admission? Does she think she knows him better than the hepatologist involved in his care over the last 4 years? Is she certain, beyond a shadow of a doubt, that he is telling the truth? Could the one admitted instance be a sign that other episodes have occurred? What triggered the ingestion of alcohol? Was it a stressful situation, indicating that Mr. Hackman turns to alcohol in times of crisis? Or was he with a group of old friends and just could not say "no," indicating that his chance of long-term sobriety may be small?
All of the above must be carefully considered in Jenny's decision. It is not as simple as it may seem. Yes, Mr. Hackman may ultimately die of complications from liver disease. People die of liver disease—an estimated 30 000 Americans annually. Not all patients receive liver transplants—only 5000 per year do. This is the harsh reality of liver transplantation. Thus, Jenny should not allow her emotions to sway her decision. Careful consideration of all the issues, particularly following discussion with the rest of the transplant team, will lead to a decision that will ultimately reap the greatest benefit for all involved.
References
- Starzl TE, Van Thiel D, Tzakis AG, et al. Orthotopic liver transplantation for alcoholic cirrhosis. JAMA. 1988;260(17):2542-2544.
- Vaillant GE. The natural history of alcoholism and its relationship to liver transplantation. Liver Transpl Surg. 1997;3(3):304-310.
- Tome S, Lucey MR. Timing of liver transplantation in alcoholic cirrhosis. J Hepatol. 2003;39(3):302-307.
- Mackie J, Groves K, Hoyle A, et al. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl. 2001;7(5):418-427.
- Burra P, Mioni D, Cillo U, et al. Long-term medical and psycho-social evaluation of patients undergoing orthotopic liver transplantation for alcoholic liver disease. Transpl Int. 2000;13(Suppl 1):S174-S178.
- Tang H, Boulton R, Gunson B, Hubscher S, Neuberger J. Patterns of alcohol consumption after liver transplantation. Gut. 1998;43(1):140-145.