Abstract
Social determinants of health are increasingly recognized as important factors in individual and public health outcomes and are therefore of interest to both health care systems and medical schools. However, teaching holistic assessment strategies during clinical education remains a challenge. This article reports on the experiences of American physician assistant students who completed an elective clinical rotation in South Africa. In particular, the students’ training and practice with 3-stage assessment is highlighted as an example of a reverse innovation practice that could be incorporated in interprofessional health care education models in the United States.
International Interprofessional Clinical Rotations
Students in US health professions programs have a strong interest in international clinical rotations. One survey of a hospital’s general surgery residents reported that 98% of respondents expressed an interest in international rotations.1 Another survey of 12 physician assistant (PA) programs noted that 60% of first-year students were interested in elective international rotations.2 A number of PA programs are offering global health pathways or tracks, typically including an elective international rotation as part of the experience,3,4 and several articles discuss how to incorporate dedicated global health tracks in PA education, including best practices for student selection and preparation.4,5
It is difficult to assess the benefits of international rotations, however. In a systematic literature review, Jeffrey et al found that medical students with international health experience reported greater confidence in their history-taking and physical exam skills and that participation increased students’ knowledge of tropical diseases and immigrant health, improved their cross-cultural awareness, and increased their likelihood of selecting high-need primary care specialties as professionals.6 Other authors have focused on ethical implications of short-term global health experiences on both host countries and medical students, including the challenges of rapidly establishing collaborations across cultures and medical systems for the benefit of patients.3 One underappreciated benefit of international rotations, however, may be the exposure of students and faculty to examples of heath care reverse innovation. One such example of reverse innovation concerns a clinical model for assessing social determinants of health (SDH): the 3-stage assessment.
Reverse Innovation
Reverse innovation describes the phenomenon of new ideas flowing from developing or emerging countries—commonly referred to as low- and middle-income countries (LMICs)—to developed, high-income countries (HICs).7 Typically, these ideas address problems common to both LMICs and HICs, but the approaches generally are less resource intensive in low-income contexts and therefore also attractive to cost-conscious, high-income countries. Although this phenomenon has been common for some time in business circles, the concept has become increasingly attractive in health care settings.8 In an analysis of 65 articles on international cooperation related to health topics, Syed et al9 identified examples of reverse innovation across the 6 World Health Organization (WHO) building blocks of health systems: “service delivery”; “health workforce”; “health information”; “medical products, vaccines, and technologies”; “health financing”; and “leadership and governance.”10 Specific examples of reverse innovation include community-based AIDS treatment programs to increase compliance that were developed in Zambia, the use of community health workers to integrate rural communities into formal health systems in Pakistan, and low-tech best practices for premature infants in Colombia.9,11
Using the WHO health systems framework, Syed et al compiled a list of 10 areas in health care for which HICs may have the most to learn from LMICs.9 Most pertinent to the experience of PA students on rotation in South Africa are the areas of rural health service delivery and creative problem solving. An example of a potential reverse innovation practice to which PA students on rotation in rural South Africa are exposed is the 3-stage assessment as a model of patient care.
3-Stage Assessment
PA clinical-year students from Concordia University Wisconsin, with which the first author (M.T.) is affiliated, first went to South Africa in 2016. The rotation is set at a district hospital in Middelburg, Mpumalanga, and largely serves a rural area as part of the government health system. As a teaching hospital affiliated with the University of Pretoria School of Medicine, it is well positioned to train PA students alongside South African medical and clinical associate students. This international elective rotation always occurs in the second half of the clinical year, allowing students to acquire necessary foundational skills prior to traveling. Beginning in 2019, the district hospital preceptors required all 4 PA students to complete a strengths, weaknesses, opportunities, and threats (SWOT) analysis upon completing the clinical rotation. The SWOT analysis was presented to students’ clinical preceptors at the district hospital and then shared with the PA program in the United States. This analysis could not be repeated in 2020, as the rotation experience was cut short by the impact of the COVID pandemic, and students were not able to return in 2021 or 2022.
Deliberate clinician focus on patients’ perspectives was remarkable to the visiting PA students.
In their SWOT, all 4 students in 2019 independently mentioned the 3-stage assessment as the greatest strength of their month-long clinical experience. The 3-stage assessment is key to the national endeavor to deliver holistic, patient-centered care within the South African health care system. The 3 distinct sections of the assessment pertain to the clinical, personal, and contextual characteristics of a patient, thereby enabling the clinician to create a comprehensive summary.12 The purpose of the summary is to facilitate collaborative, interprofessional, multisectoral management of patients, in particular at times of referral and discharge.12 During the rotation, the entire 3-stage assessment was clinician led, including the personal and contextual sections, and was a regular focus during the morning clinical meetings when care of the patients in the wards was discussed. It is this deliberate clinician focus on patients’ perspectives on their illness and treatment—as well as patients’ living arrangements, livelihood, and dependents—that was remarkable to the visiting PA students.
In the facility where they train, PA students are instructed on 3-stage assessment during the first day of the rotation and then expected to use it with patients during their month-long elective. Review of the 4 individual SWOT analyses at the end of the 2019 rotation identified several common themes: all 4 students noted the prominent role of holistic assessment by South African physicians as a major strength of their rotation experience, with 3 of the students mentioning “3-stage assessment” by name, and the fourth student describing all 3 components of the assessment. All 4 students noted that they had not been taught or applied an equivalent social assessment model during their prior 6 clinical rotations in the United States. And all 4 students mentioned the utility of bringing social aspects into clinical discussions via simple conversations that addressed barriers to follow-up appointments or child care considerations. Finally, all 4 students had positive overall impressions of 3-stage assessment, describing the process as “a large benefit” or “incredibly rewarding” or stating that it “will help make me a better provider when I return home to the United States.” Students’ reflections on 3-stage assessment from their SWOTs are displayed in the Table.
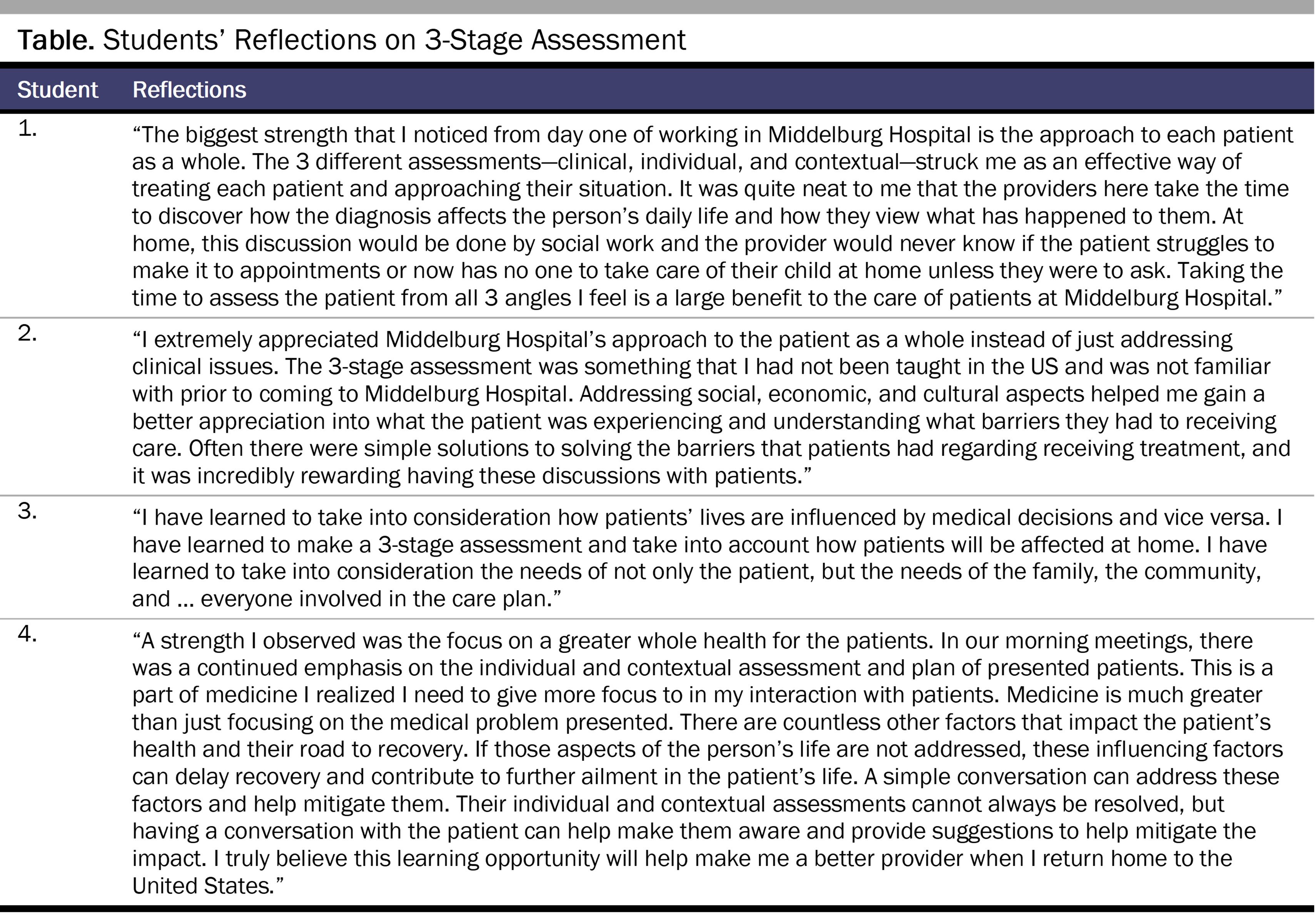
However, it was the deliberate implementation of this model with every patient, both initially and on an ongoing basis, that made such an impression on students and was therefore viewed by them as unique in their health care experience. The 4 students’ reflections suggest that IPE classes and events would benefit from allowing PA students to fully participate in the personal and contextual aspects of patient care instead of delegating these aspects to nursing or social work colleagues.
Conclusion
Over the past 20 years, US medical schools and PA programs have become aware of the need to approach patients more holistically, often addressing this need through curricular redesign that incorporates a greater emphasis on SDOH.13 In clinical practice, US clinicians are often unable to complete SDOH assessments with their patients, however. Schickedanz et al found that though 84% of surveyed health care professionals supported screening for SDOH, only 41% reported confidence in their ability to conduct such screenings, and only 23% reported routinely screening for SDOH due to “lack of training,” “lack of time,” and “lack of resources to address any social needs identified,” with these barriers felt most acutely by physician respondents.14 Therefore, identification of promising and potentially cost-saving holistic health models used in international health systems, such as 3-stage assessment, is important for removing these barriers. If future student reflections on using the 3-stage assessment in South Africa are as strongly positive as those of the 2019 student cohort, it would suggest that US health care educators might benefit from learning about this model and seeing if it could be adapted to clinical education and practice. If so, 3-stage assessment would serve as an example of reverse innovation in health care.
Syed et al emphasize that a critical step in reverse innovation is a strong commitment to valuing innovative ideas or technologies,9 and one way to promote this commitment is through research. The 3-stage assessment is a fundamental component of the South African medical system, and its impact on care and care coordination in South Africa is being studied.12,15 Concordia University Wisconsin’s 4 years’ experience with PA clinical year rotations in South Africa suggests additional lines of research. Study on this topic could include both ongoing review of SWOT analyses of future PA students traveling to South Africa, especially their attitudes toward 3-stage assessment, as well as assessment of PA graduates’ ability to implement in US practice settings the social aspects of care they were exposed to in South Africa, with a particular focus on the challenges they experience in implementation.
References
- Powell AC, Mueller C, Kingham P, Berman R, Pachter HL, Hopkins MA. International experience, electives, and volunteerism in surgical training: a survey of resident interest. J Am Coll Surg. 2007;205(1):162-168.
- Luce D, Stewart N, Davison M. Physician assistant studentsʼ attitudes toward international experiences. J Physician Assist Educ. 2007;18(2):14-20.
- Crump JA, Sugarman J. Ethical considerations for short-term experiences by trainees in global health. JAMA. 2008;300(12):1456-1458.
- Davis-Risen S, Backman R. Global health tracks in physician assistant education: making the case. J Physician Assist Educ. 2017;29(2):164-166.
-
Nelson M. How to develop an international clinical rotation. Physician Assistant Education Association. August 12, 2015. Accessed January 20, 2021. https://paeaonline.org/resources/public-resources/paea-news/develop-an-international-clinical-rotation
- Jeffrey J, Dumont RA, Kim GY, Kuo T. Effects of international health electives on medical student learning and career choice: results of a systematic literature review. Fam Med. 2011;43(1):21-28.
-
Depasse JW, Lee PT. A model for “reverse innovation” in health care. Global Health. 2013;9:40.
-
Khan M. 20 inspirational reverse innovation examples in business. Insight and Innovation. January 23, 2022. Accessed December 6, 2022. https://insightandinnovation.com/20-inspirational-reverse-innovation-examples-in-business
-
Syed SB, Dadwal V, Rutter P, et al. Developed-developing country partnerships: benefits to developed countries? Global Health. 2012;8:17.
-
World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. World Health Organization; 2010. Accessed January 20, 2021. https://apps.who.int/iris/bitstream/handle/10665/258734/9789241564052-eng.pdf?sequence=1&isAllowed=y
- Kangovi S, Grande D, Trinh-Shevrin C. From rhetoric to reality—community health workers in post-reform US health care. N Engl J Med. 2015;372(24):2277-2279.
- Hugo JFM, Maimela TCR, Janse van Rensburg MNS, Heese J, Nakazwa CE, Marcus TS. The three-stage assessment to support hospital-home care coordination in Tshwane, South Africa. Afr J Prim Health Care Fam Med. 2020;12(1):e1-e10.
-
Hinote B, Wasserman J. The illness experiences of patients and families. In: Social and Behavioral Science for Health Professionals. Rowan & Littlefield; 2020:178-199.
- Schickedanz A, Hamity C, Rogers A, Sharp AL, Jackson A. Clinician experiences and attitudes regarding screening for social determinants of health in a large integrated health system. Med Care. 2019;57(6)(suppl 2):S197-S201.
-
Draper C, Smith P. Psychiatry in primary care using the three-stage assessment. S Afr Med J. 2013;104(1):74.