Abstract
Since the Joint Commission shifted its focus to suicide mitigation strategy implementation in behavioral health units in 2007, examining modern design trends in historical context is more clinically and ethically important than ever. This article considers architectural evolutions in how health care organizations have used structure and space designs to balance safety and healing when housing patients who are suicidal.
History of Psychiatric Inpatient Unit Design
An intimate history of psychiatry and architectural design has been forgotten with the advent of modern psychiatric treatment and medications. However, the 19th century saw the emergence of psychiatry as a medical specialty and tremendous growth of and investment in asylums for those with mental illness.1,2 Psychiatrists during this period relied on specially designed asylums not merely to house patients but as a core part of treatment.1 It was believed that 70% to 90% of individuals with psychiatric conditions were curable, provided they left home to receive treatment in purposefully structured asylums.1 Daylight and ventilation were prioritized in building design, with the first few asylums focused on having corridors with rooms on one side and a shared indoor walkway on the other side.1 In comparison to the more economical option of having corridors with rooms on both sides, these single-loaded corridors allowed fresh air and light to freely pass from the exterior of the building to the patient room. The Kirkbride, or linear, plan quickly became the exemplary model for asylum design.3 It was composed of a series of small, interconnected buildings arranged in a shallow V (see Figure), which granted all patients an unhindered outside view of the natural landscape as well as ventilation. However, its layout inadvertently became associated with patient hierarchy, with the loudest and most troublesome patients allocated to the building’s outskirts and further removed from physician care.1
Figure. Lithograph of Kirkbride Design Blueprint for Trenton State Hospital, circa 1848
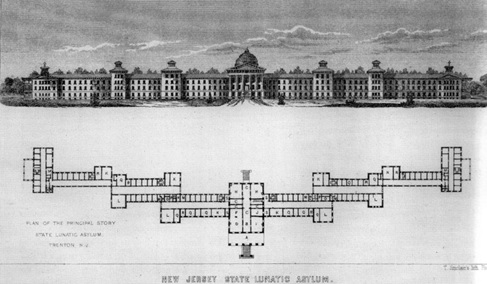
Note: Follows principles of Kirkbride plan by including short, interconnected buildings featured in a V shape.
Contemporary Shifts Toward Emphasis on Architecture
Fast forward to our modern era. While the pages of psychiatry journals were once filled with a focus on buildings, psychiatric treatment now is centered on medications.4 However, the renewed influence of architectural design on psychiatry is apparent in 2 competing goals of care.
Reducing risk. The Joint Commission (TJC)—which started regulating psychiatric hospitals on the same basis as medical ones in the 1990s5—began to focus on environmental threats to patient safety in 2007, when it declared a National Patient Safety Goal of preventing suicides on inpatient units,6 given the widely cited statistic of 1500 inpatient suicides per year in the United States.7 This statistic was initially published in the American Psychiatric Association (APA) 2003 clinical practice guidelines, with the further remark that one-third of suicides occurred despite one-on-one patient observation or 15-minute checks.7 In response, psychiatric hospitals adhering to the new TJC guidelines were required to make large design changes to mitigate suicide risk.
The widely cited 1500 inpatient suicides per year statistic remained undisputed until an in-depth investigation published in a TJC journal revealed that the actual number of inpatient suicides ranged from 48.5 to 64.9 per year, vastly lower than the previously suggested 1500.8 It appears that the original figure was an estimate without any basis in actual data, and yet it has had a profound effect on regulatory policy. Furthermore, it has been well documented that significantly more suicides occur following discharge from inpatient psychiatric hospitalization than during hospitalization.8 This information forces us to reconsider at what cost to the health care system and patients we are changing built environments on the mistaken assumption that suicide risk mitigation should be prioritized over other design goals.
The quality of staff-patient and patient-patient social interactions can enrich a patient’s experience on psychiatric wards and create a less stigmatizing social environment.
Healing power of the environment. In the last few decades, there has been a renewed interest in the impact of general hospital design on patient outcomes across all medical specialties. Ulrich’s transformative paper, published in 1984, asserted that post-cholecystectomy patients staying in rooms with window views of nature had a shorter average length of stay than those in windowless rooms.9 Similar associations between patient outcomes and room design can be found in the psychiatric literature. One study found that less anxiety medication was dispensed by nurses on a psychiatric unit when realistic nature artwork was hung on the wall than when abstract or no art pieces were displayed.10 Similarly, an intensive care unit study evaluating the benefit of daylight for delirium found that delirious patients in rooms with windows had fewer behavioral episodes warranting antipsychotics than those in windowless rooms.11
While the effect of architectural design on mental health deserves further study, we know the significance of this relationship extends beyond hospital walls. Encouraging findings have emerged from studies evaluating the association between physical environment factors and behavioral outcomes. For example, a systematic review of the relationships among urban green space, violence, and crime revealed that though the results were mixed, “more evidence support[ed] the positive impact of green space on violence and crime, indicating great potential for green space to shape health-promoting environments.”12 It is important to note that the relationship between architecture and health outcomes is likely not confined to the effects of one or two design variables. Instead, it is the creation of a built environment focused on room layout, furniture, interior design, and wayfinding that produces therapeutic spaces.
Conflicting Priorities
While the general rekindled interest in the relationship between hospital design and patient outcomes is encouraging, with respect to the design of psychiatric facilities, there is a tug of war between proponents of creating a healing environment and proponents of minimizing suicide risk. It is difficult to discern whether these 2 priorities are mutually exclusive or can be equally, effectively, and concomitantly addressed with thoughtful design. Given that hanging is the predominant method of suicide in the inpatient setting, TJC has prioritized mitigating ligature risk in its suicide safety standards.8 However, there has been widespread uncertainty regarding the implementation of these vague guidelines and the cost of renovations. The requirement for hospitals to be as ligature free as possible has been accompanied by minimal instruction from TJC on how to implement this standard in the physical space, and implementation has been further impeded by a limited number of design furniture vendors for behavioral wards. The APA found that, in 2017, 23 facilities reported paying between $6 million and $100 million for ligature-risk citations, and 14 hospitals had been forced to reduce their number of psychiatric beds.13 Thus, facilities have been cited for issues related to suicide risk and pressured to make changes that are not feasible due to physical barriers and cost, despite TJC surveyors having limited evidence to inform their practices. While there have been attempts to reduce suicide rates using mental health checklists, the impact of these checklists is unclear, given the small number of completed suicides on inpatient psychiatric units.14 As such, it has become common practice for medical directors of psychiatric facilities to hire consultants to inspect hospitals before official TJC surveys to interpret how these ambiguous guidelines apply to their physical spaces. An example of one such consultation occurred on our adult inpatient psychiatric unit, where a piano and uncaulked paintings in the common space were identified as potential ligature risks.
Psychiatric wards differ from general medical units in their use of public spaces to provide opportunities for positive social engagement.15 It is well established that the quality of staff-patient and patient-patient social interactions can enrich a patient’s experience on psychiatric wards and create a less stigmatizing social environment.15 Key design features—including a homelike environment with a diversity of communal spaces, open nursing spaces, and mobile furniture that can be arranged in small, flexible groupings—have been shown to promote positive interactions.16 Outdoor public spaces with access to nature can also elevate patient physical and mental well-being.17 In contrast, a poorly designed environment void of stimuli and comfort can limit cognitive function and contribute to patients feeling stigmatized due to their struggles with mental health.15,18 This distinction between well and poorly designed environments becomes important especially when consultants advise removing communal objects (such as the piano in the example above) or adjusting furniture in public spaces without consideration of how design elements contribute to the healing and building of a larger community. This trade-off between safety and healing is also apparent in modern behavioral health furniture, which is generally designed to minimize safety risks rather than to promote aesthetics, comfort, or mobility.
Of note, the safety-healing trade-off is most apparent in public spaces, as 90% of inpatient suicides occur in private spaces, including the bedroom, bathroom, closet, and shower.8 Given the burden of suicides in private spaces, it would be worthwhile to consider how suicide risk mitigation strategies, along with staff-to-patient ratio, should differ in public and private spaces. Standardized suicide prevention guidelines could be developed that consider characteristics of a unit’s physical space, with relatively greater emphasis on risk mitigation in private spaces in the least intrusive manner possible. Where renovation or new construction of inpatient psychiatric units is considered, thoughtful design would ideally foster the creation of healing spaces in both private and public areas while minimizing safety risks.
Balancing Safety and Healing
In addition to implementing design elements to mitigate suicide risk in inpatient psychiatric units, organizations (both health care and accreditation), researchers, and clinicians should also keep in mind the potential of architectural design to create healing spaces. TJC guidelines have largely narrowed the focus to interventions on the built environment that theoretically minimize acute suicide risk. However, these interventions not only lack empirical support but also prioritize risk management over healing. To balance the promotion of therapeutic spaces with reduction of safety risks, TJC guidelines for psychiatric hospitals could be modified to distinguish between public and private spaces based on the different hazards associated with each location. As mentioned, research has shown that suicides occur predominantly in private spaces; aggression, inappropriate behavior, and falls occur in both private and public spaces.19 Thus, TJC ligature risk-based guidelines could focus on private spaces while TJC supervision-based guidelines (eg, for clear views of communal spaces and corridors from the central nursing area) could focus on public spaces. However, it is essential to recognize that adverse incidents can often be reduced or prevented with environmental adaptations geared toward healing. Designing public spaces with the intent of reducing noise and stress from crowding (eg, movable furniture) or offering positive distractions (eg, nature art) can reduce incidents of aggressive behavior.20 The physical environment is also a known contributor to falls, with documented risk factors that include poor nighttime lighting, uneven floors, and spaces that limit visual observation.21 Thus, design interventions for public spaces that provide clear views, reduce overstimulation, promote engagement (eg, via diversity of communal areas with movable seating), and offer positive distraction (via nature artwork, windows with nature views, and ample daylight) better align with the therapeutic value of recovery and could still mitigate fall risks in contradistinction to design interventions for private spaces, which largely focus on structural ligature risk-reducing interventions. Such design elements have been shown to contribute to positive healing in psychiatric patients.17,20,22 Instead of enforcing stringent ligature risk regulations in private and public spaces, TJC should consider partnering with health care organizations and behavioral health units in revising current guidelines to strengthen the therapeutic qualities of spaces.
As former National Institute of Mental Health director Thomas Insel has pointed out, there is substantially more to healing from mental illness than is incorporated in our current practice.23 We must remember that treating patients’ underlying mental illness and providing them with tools to cope with distressing emotions and adverse circumstances are the most effective methods in suicide prevention.24 Health care organizations contemplating restructuring of their behavioral unit should consider incorporating known therapeutic design elements—privacy, sound reduction, daylight, environmental complexity, ventilation, color, and nature—while also incorporating opportunities for clinicians to observe patients (eg, open nursing units) to help maintain patient autonomy.17,22 Instead of seeing the environment as something patients need protection from, we should regard physical spaces as another nonpharmacological strategy to add to our tool kit for the prevention and treatment of psychiatric conditions.
References
-
Yanni C. The Architecture of Madness: Insane Asylums in the United States. University of Minnesota Press; 2007.
-
Grob GN. Mental Illness and American Society, 1875-1940. Princeton University Press; 1983.
-
Tomes N. The Art of Asylum-Keeping: Thomas Story Kirkbride and the Origins of American Psychiatry. University of Pennsylvania Press; 1994.
-
Grob GN. The Mad Among Us: A History of the Care of America’s Mentally Ill. Harvard University Press; 1994.
-
Joint Commission on Accreditation of Healthcare Organizations. Accreditation Manual for Hospitals. The Commission; 1992.
-
Thom R, Hogan C, Hazen E. Suicide risk screening in the hospital setting: a review of brief validated tools. Psychosomatics. 2020;61(1):1-7.
- American Psychiatric Association Steering Committee on Practice Guidelines. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11)(suppl):1-60.
- Williams SC, Schmaltz SP, Castro GM, Baker DW. Incidence and method of suicide in hospitals in the United States. Jt Comm J Qual Patient Saf. 2018;44(11):643-650.
- Ulrich RS. View through a window may influence recovery from surgery. Science. 1984;224(4647):420-421.
- Nanda U, Eisen S, Zadeh RS, Owen D. Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. J Psychiatr Ment Health Nurs. 2011;18(5):386-393.
-
Smonig R, Magalhaes E, Bouadma L, et al. Impact of natural light exposure on delirium burden in adult patients receiving invasive mechanical ventilation in the ICU: a prospective study. Ann Intensive Care. 2019;9(1):120.
- Bogar S, Beyer KM. Green space, violence, and crime: a systematic review. Trauma Violence Abuse. 2016;17(2):160-171.
-
Moran M. Report shows number of hospital suicides lower than estimated. Psychiatry News. October 12, 2018. Accessed March 28, 2023. https://psychnews.psychiatryonline.org/doi/full/10.1176/appi.pn.2018.10b10
- Watts BV, Shiner B, Young-Xu Y, Mills PD. Sustained effectiveness of the Mental Health Environment of Care Checklist to decrease inpatient suicide. Psychiatr Serv. 2017;68(4):405-407.
-
Molin J, Graneheim UH, Lindgren BM. Quality of interactions influences everyday life in psychiatric inpatient care—patients’ perspectives. Int J Qual Stud Health Well-being. 2016;11(1):29897.
-
Jovanović N, Campbell J, Priebe S. How to design psychiatric facilities to foster positive social interaction—a systematic review. Eur Psychiatry. 2019;60:49-62.
-
Hjort M, Mau M, Høj M, Roessler KK. The importance of the outdoor environment for the recovery of psychiatric patients: a scoping review. Int J Environ Res Public Health. 2023;20(3):2240.
-
Davidson AW, Bar-Yam Y. Environmental complexity: information for human-environment well-being. In: Minai AA, Bar-Yam Y, eds. Unifying Themes in Complex Systems: Proceedings of the Third International Conference on Complex Systems. 2006:157-168.
- Bayramzadeh S. An assessment of levels of safety in psychiatric units. HERD. 2016;10(2):66-80.
-
Ulrich RS, Bogren L, Gardiner SK, Lundin S. Psychiatric ward design can reduce aggressive behavior. J Environ Psychol. 2018;57:53-66.
- Bayramzadeh S, Portillo M, Carmel-Gilfilen C. Understanding design vulnerabilities in the physical environment relating to patient fall patterns in a psychiatric hospital: seven years of sentinel events. J Am Psychiatr Nurses Assoc. 2019;25(2):134-145.
- Schweitzer M, Gilpin L, Frampton S. Healing spaces: elements of environmental design that make an impact on health. J Altern Complement Med. 2004;10(suppl 1):S71-S83.
-
Insel T. Healing: Our Path From Mental Illness to Mental Health. Penguin Press; 2022.
- Mann JJ, Michel CA, Auerbach RP. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry. 2021;178(7):611-624.