Abstract
Inquiry-based learning instructional design methods support online health professions capability-based curricula. This article proposes which instructional design priorities should guide development of inclusive, accessible online curricula and learning experiences.
Inquiry-Based Learning
In this article, we explore instructional design strategies related to inquiry-based learning (IBL) for online, or virtually mediated, health professions education. IBL is characterized by individual and team-based development and supports analytical reasoning through exploration and stimulating curiosity. We focus primarily on how such strategies have the potential to support online capability-based curricula that emphasize self-awareness and reflection in particular patient-care contexts to afford an accessible and inclusive learning environment.
Cultivating Capability
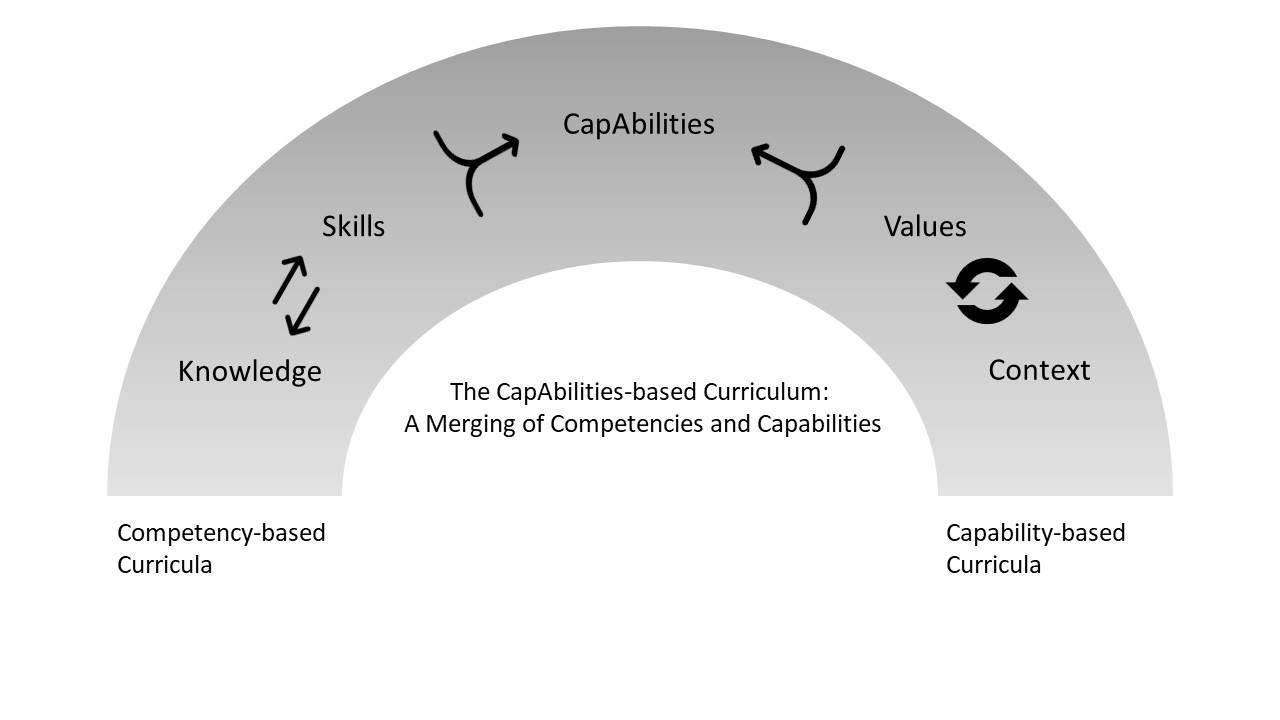
We begin by providing some context in relation to capability-based curricular design, given that health professions education has primarily adopted competency-based curricula, which are designed so that learning can be assessed by measuring particular outcomes (competencies).1 Whereas competency-based curricula aim to teach observable abilities (eg, to diagnose and treat illness), capability-based curricula aim to support the development of professionals who can not only provide a medical diagnosis but also situate that diagnosis within the wider life of the patient.2,3 Although a competency-based curriculum does aim to account for a comprehensive set of attributes, it tends to reduce lived experience to “lists of attributes ... that exoticize patients, ultimately obscuring social context, medical culture, and structures of power.”4
If competency-based curricula focus on the science of medicine, capability-based curricula focus on the art of medicine.5 In particular, capability-based curricula encourage and challenge both instructors and students to explore previously unexamined beliefs and assumptions that influence their behaviors as health professionals. Capability-focused physicians would not just administer the right medicines and treatment plan; they would work with the patient to identify the most suitable pharmacy for pickup or delivery according to the patient’s needs or try to schedule back-to-back referral appointments if they were aware that the patient is unable to keep medical appointments without taking time off from work. In other words, a capability-focused physician cultivates a holistic awareness of the patient in context. Such an awareness is considered to be an art rather than a science.5 It necessitates that health professionals reflect on their assumptions about patient care and the kinds of questions they ask and fail to ask patients; foster an awareness of the patient’s ailment; and recommend treatment that not only meets the patient’s medical needs (science) but also is tailored to the patient’s lived reality (art). In other words, a capability-based curriculum seeks to support the development of a health professional who is focused on patient care.
A capability-based curriculum does not detract from a competency-based curriculum but rather enhances it. By enhancing competencies with capabilities, the curriculum design approach becomes a holistic one (see Figure 1). For competency-based curricula, instructional design methods for online environments emphasize didactic materials and knowledge acquisition. For capability-based curricula, the emphasis shifts to strategies that enable inquiry in order to facilitate the learner’s awareness of the learning process. Presently, there is a large body of literature related to designing online competency-based curricula.6,7,8,9,10,11,12,13 Little has been written about designing capability-based curricula for online medical education, however. The rest of the article elaborates on the latter.
Figure 1. The Capabilities-Based Curriculum: A Merging of Competencies and Capabilities
Postures for Online Capability-Based Learning
Rather than focusing on observable skills, capability-based curricula aim to foster postures that enable building patient-centered awareness. The 3 postures that we address in this article are radical relationality, collective knowledge building, and critical self-reflection.14,15,16,17 We generated these postures from examination of other disciplines—including disability studies, social justice education, and feminist studies—that aim to foster learners’ critical consciousness.2,16,18,19 Before we connect these postures to concrete design strategies, we define them below.
Radical relationality. This posture is adapted from Veletsianos and Houlden’s concept of radical flexibility.14 In relation to learning and caring, radical relationality involves seeing all individuals as connected to one another and considering the multiple and changing roles and responsibilities that exist due to this connection. Individuals have rich histories and experiences that have shaped and continue to shape them throughout their lives. Radical relationality recognizes this interconnectedness and calls for responsibility on the part of the clinician to provide life-sustaining and life-supporting care reflective of the reality of each unique individual.14 A professional practicing radical relationality would ask patients about not only the nearest pharmacy but also how they feel about taking medicine or if they have cultural beliefs that inform their approach to receiving medicine.
Collective knowledge building. For collective knowledge building to occur, medical education must be seen not as a one-way transmissible process but rather as a nonhierarchical discovery process in which students and educators collectively generate answers to problems.15,16,19 Educators become problem posers and enable learners to think critically about medical issues.15 Ideally, a collective knowledge-building approach to clinical care is one in which a physician might invite patients to raise questions about their health care or to create mutually agreeable short-term goals.15 Such a posture might enable students to recognize patients as playing a vital role in their own health.
Critical self-reflection. Through reflection, one engages in self-probing approaches to gain insight that can aid one’s professional development.20 In critical pedagogy, the posture of critical self-reflection involves assessing one’s personal beliefs and personal and professional interactions so that one becomes aware of the various inequities that are present in the lives of one’s patients, society, and medicine as a whole; how personal biases can influence patient care; or even how professionals can support one another in cases of less-than-optimal outcomes (eg, uncooperative patients or inopportune circumstances).16, 17, 19 Through critical reflection, educators and students can foster empathy, examine their assumptions to manage their biases, and commit to practices that provide equitable outcomes for those they serve.
To weave these postures into online health professions education, we focus on IBL strategies.
Why IBL Is Key to Online Capability-Based Learning
With the rise of online education since the early 2000s, there has been increasing interest in more human-centered instructional strategies. IBL emphasizes a problems-first approach, starting with an examination of what the problem might be. The design of IBL activities tends to follow a sense-making process that allows for exploration in problem identification and strategy formation. According to Lim, in order for “inquiry to be meaningful, the topics need to be developed based on the learners’ needs and capabilities.”21 IBL accommodates this tailored approach to inquiry by enabling the addition of new approaches or the adaptation of existing ones as needs arise.
IBL can be thought of as the umbrella framework that includes more specific methods, such as problem-based learning (PBL), project-based learning, and design-based learning.22
PBL became prominent in medical education curricula that focus on the development of both individual critical thinking and clinical skills and team-based development.23 IBL as the method of choice to support critical problem-solving skills has the added advantage of enabling a more holistic and flexible reasoning process. For example, instead of starting a sequence of online activities with a lecture, the curricular design would begin with an exploratory activity, such as an online poll asking learners to select a response to a complex scenario, followed by a brief write-up of the justification of that selection. Once a learner submits this information, immediate feedback would be provided in relation to what their peers have also selected and justified, inviting learners to reconsider their response or justification. Starting with inquiry that fosters the postures of collective knowledge building and critical self-reflection allows learners to become active participants in their learning process.
Similar to a learner’s reasoning being enhanced by awareness of peers’ perspectives, making the right prescription requires understanding of context—here, the context surrounding the patient’s ability to obtain the prescribed medication based on cost or physical or logistical issues (the posture of radical relationality). It is therefore important to design medical education curricula that focus on the development of capabilities based on the 3 postures. Using IBL as the design framework with a focus on the sense-making process allows interrogation of the instructional strategies we currently use and exploration of strategies that we should consider using in capability-based medical education.
Consider the following sense-making model24,25 shown in Figure 2. This model focuses on the types of cognitive processes that take place as part of problem-solving activities: exploration, followed by identification, processing/reasoning, judgment, and integration, all of which are enhanced by the 3 postures. It represents the sense-making process as a dynamic cycle that culminates in the integration of knowledge. What this model enables us to do is to consider activities that merge instructional and learning strategies.
Figure 2. Reflective Sense-Making Learning Model
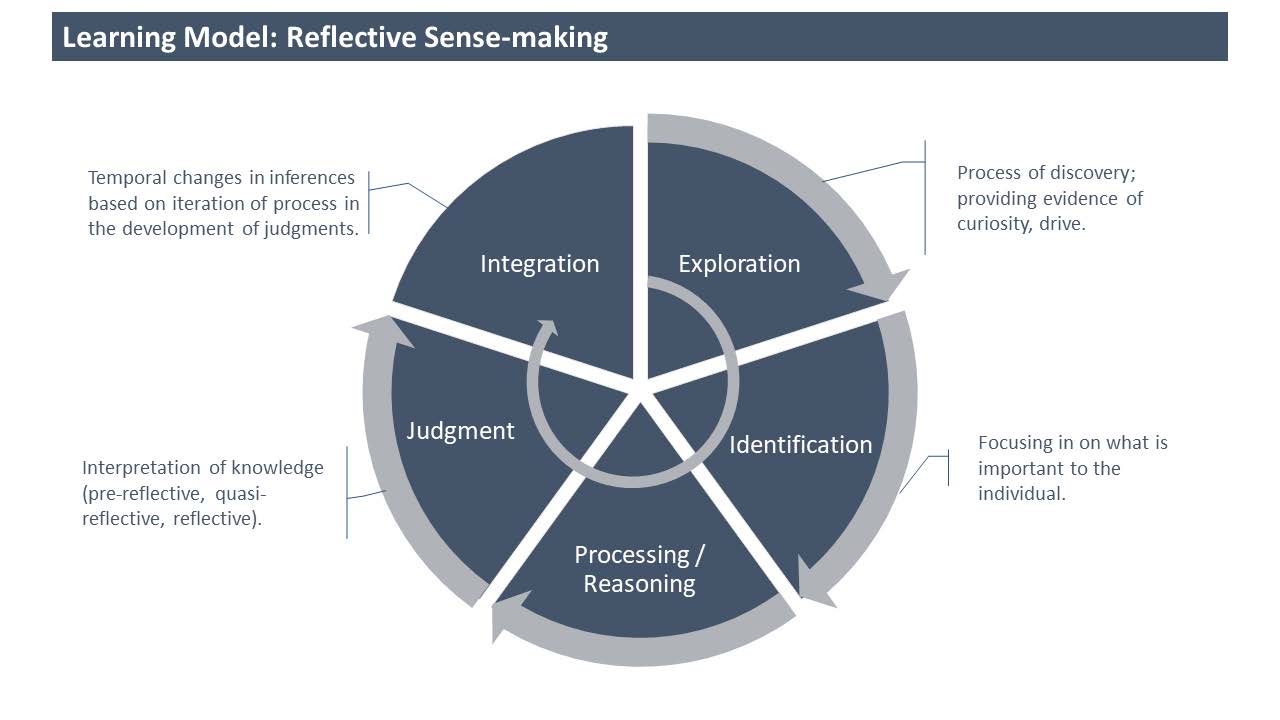
Text adapted from Lotrecchiano et al.24
The IBL strategies we believe align postures and components of the sense-making process are the following: questioning, pattern spotting, and adaptive actioning. These strategies are drawn from the field of human systems dynamics, which is grounded in inquiry-based methods that have been tested in online learning environments.
- Questioning. Questioning has been widely used across disciplines to foster critical thinking about subject matter knowledge.26 According to Tofade et al, “well-crafted questions lead to new insights, generate discussion, and promote the comprehensive exploration of subject matter.”27 To support capability development, we also need to focus on using questioning strategies that enable identification, a sense of connection “to some external entity (such as an idea, philosophy, person, group, or organization) that gives some measure of meaning to their identity.”28 By doing so, we are more likely to enable critical self-reflection.
- Pattern spotting. Pattern spotting emerged from research on complex adaptive systems.29 It is a type of processing/reasoning that involves recognizing patterns by identifying differences, similarities, and connections when trying to make sense of ill-structured problems. Through inquiry, we can home in on the challenges that emerge within a particular space by noticing differences and similarities between current and past problems. By doing so, we are more likely to enable collective knowledge building.
- Adaptive actioning. Adaptive actioning flows from pattern spotting. While pattern spotting involves analysis of the past and present, adaptive actioning enables us to consider what actions to take in the future, which takes judgment,30 and in turn enables critical self-reflection.
IBL Strategies in Action
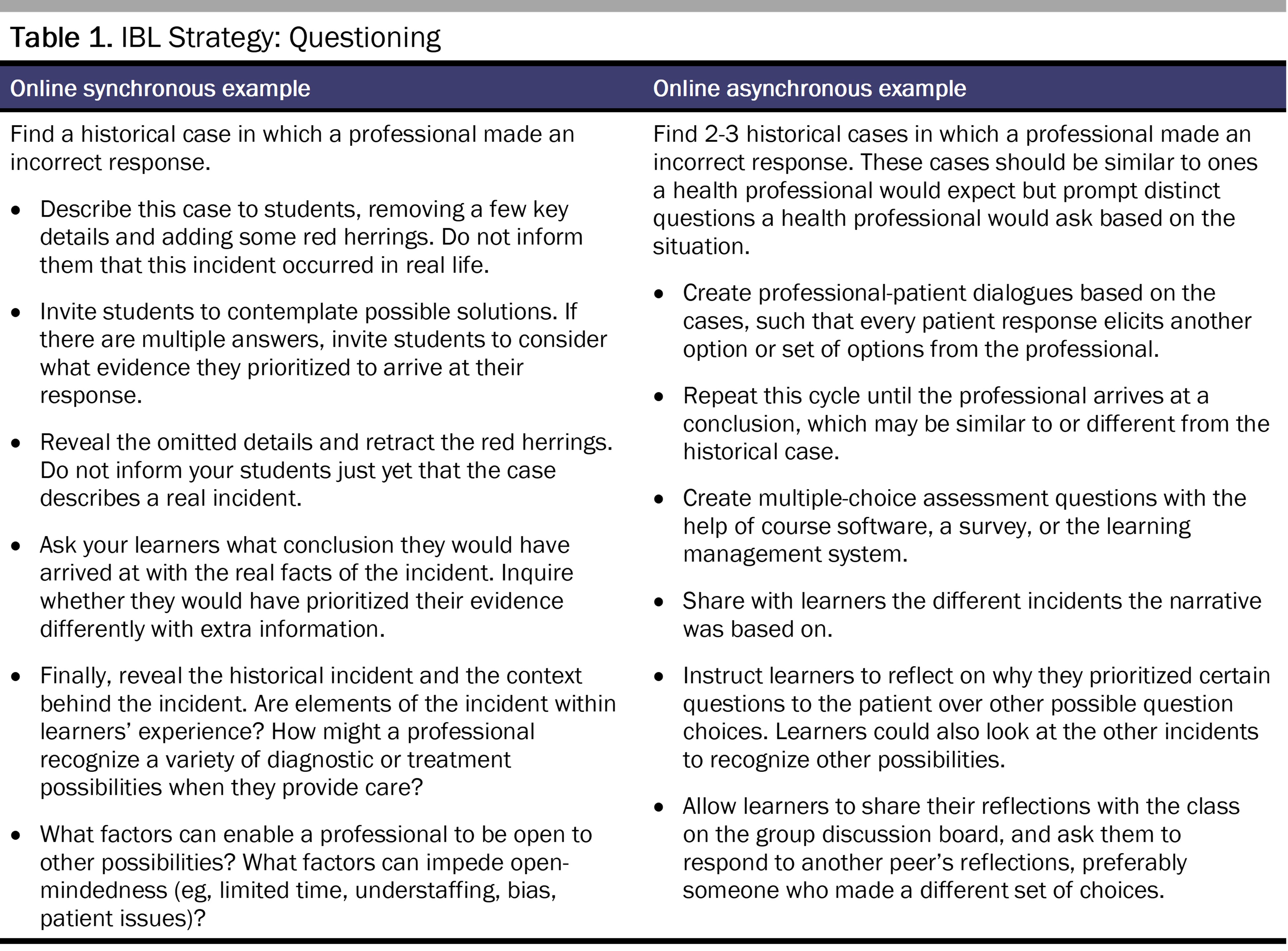
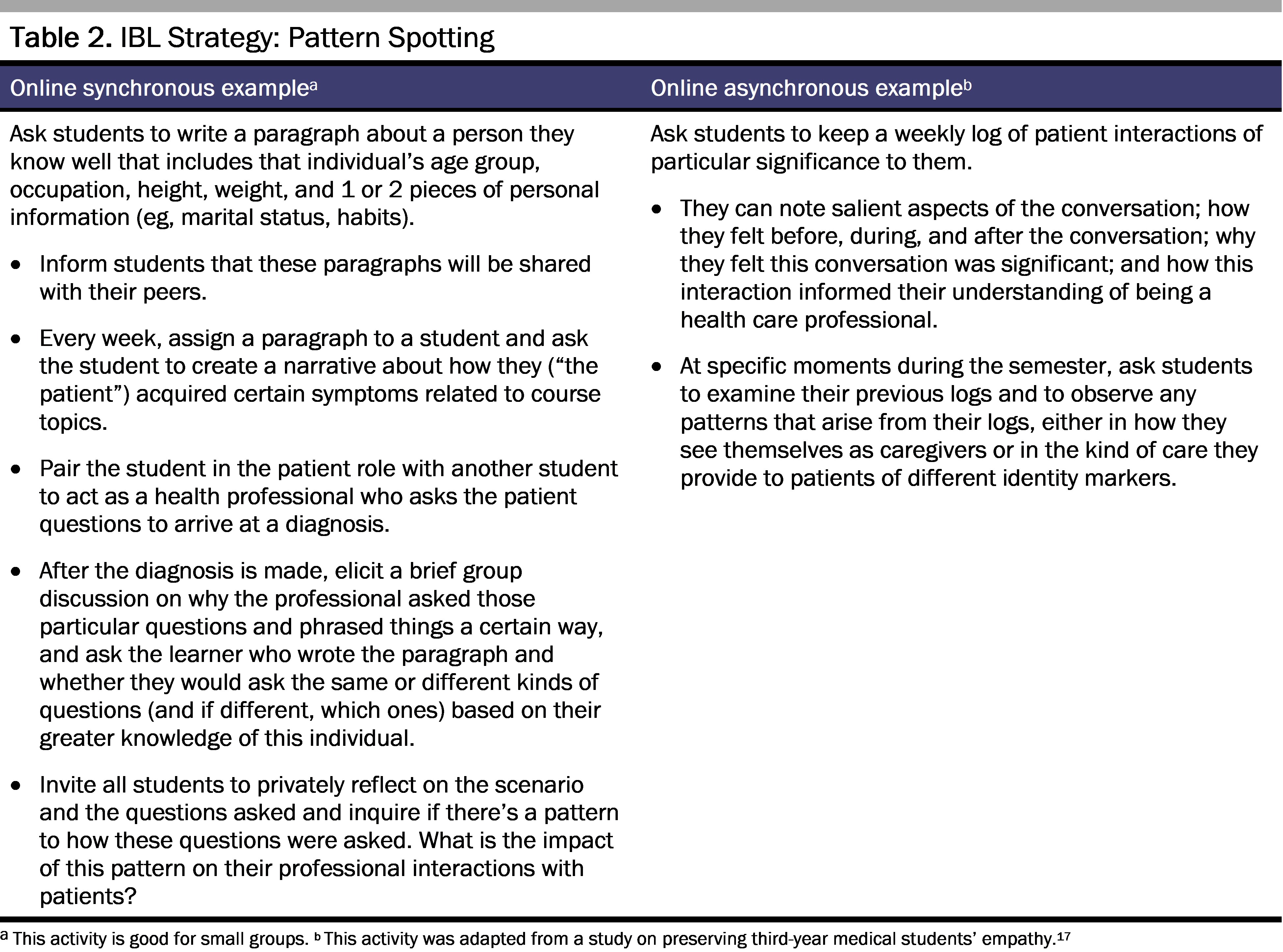
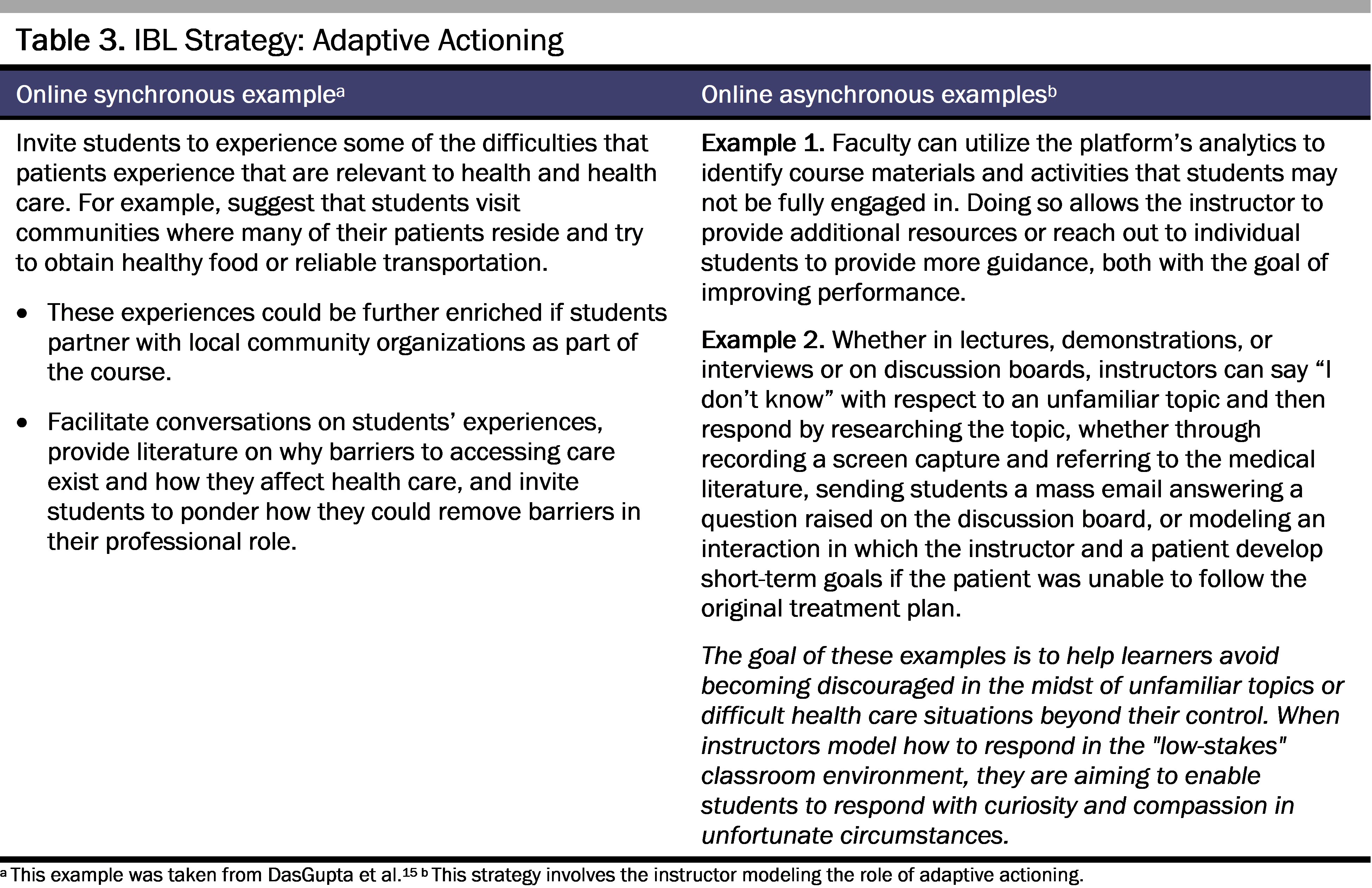
We offer the following guidance to make design decisions with intention that will support an inclusive online teaching and learning environment. Tables 1, 2, and 3 present the IBL strategies, along with guiding questions that are aligned with the postures essential to building patient-centered awareness. In addition to these questions, we present examples through which instructors can foster the exploration of these questions in an online course, either in real time (synchronous) or outside class time (asynchronous). While these examples are adapted to health professions education, several of them are based on educational interventions from other disciplines.18,19,31,32,33,34,35,36,37,38,39
IBL Strategy 1: Questioning. What are you assuming about this patient that might not be true?40,41
IBL Strategy 2: Pattern spotting. Do I assume different outcomes because of a patient’s race, ethnicity, sexuality, or linguistic background?42
IBL Strategy 3: Adaptive actioning. How might you derive value from a situation involving a bad outcome?
Conclusion
In capability-based curricula, instructional design emphasizes understanding contextual factors that influence individuals as well as factors that influence how the work gets done within an organization. This design enables an examination of values held at both the individual and the organizational level (ie, nonobservable attributes). The awareness of context and values influences students’ approach to and success in developing their capabilities.
In design of online capability-based curricula, we propose a model that synthesizes a competencies approach based on outcomes and a capabilities approach based on cognitive processes through theoretical and practical applications. In this proposed reflective sense-making model, students are trained to recognize symptoms and provide treatment to patients (competencies) while also situating patients’ health in their lived experience (capabilities). Through application of the 3 IBL strategies, educators can help students foster postures that promote patient-centered awareness. This holistic awareness, in turn, enables students to better understand the lived reality of their patients and the unique factors that promote or impact their health, as well as to tailor treatment to the individual.
Our future research aims to explore how both competency-based and capability-based curricular design approaches can come together. We hope to examine this framework in relation to online learning within the context of medical education and identify more IBL strategies that support the postures of radical relationality, collective knowledge building, and critical self-reflection, which in turn enhance learning of capabilities.
References
- Ryan MS, Holmboe ES, Chandra S. Competency-based medical education: considering its past, present, and a post-COVID-19 era. Acad Med. 2022;97(3S):S90-S97.
- Walker M. Towards a capability-based theory of social justice for education policy-making. J Educ Policy. 2006;21(2):163-185.
- Kumagai AK, Lypson ML. Beyond cultural competence: critical consciousness, social justice, and multicultural education. Acad Med. 2009;84(6):782-787.
- Dao DK, Goss AL, Hoekzema AS, et al. Integrating theory, content, and method to foster critical consciousness in medical students: a comprehensive model for cultural competence training. Acad Med. 2017;92(3):335-344.
- Saunders J. The practice of clinical medicine as an art and as a science. Med Humanit. 2000;26(1):18-22.
-
Power JE, Toft LEB, Barrett M. The murmur online learning experience (Mole) curriculum improves medical students’ ability to correctly identify cardiac murmurs. MedEdPORTAL. 2020;16:10904.
- Mao BP, Teichroeb ML, Lee T, Wong G, Pang T, Pleass H. Is online video-based education an effective method to teach basic surgical skills to students and surgical trainees? A systematic review and meta-analysis. J Surg Educ. 2022;79(6):1536-1545.
-
Regmi K, Jones L. A systematic review of the factors—enablers and barriers—affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):91.
-
Sajid MR, Laheji AF, Abothenain F, Salam Y, AlJayar D, Obeidat A. Can blended learning and the flipped classroom improve student learning and satisfaction in Saudi Arabia? Int J Med Educ. 2016;7:281-285.
- Jayakumar N, Brunckhorst O, Dasgupta P, Khan MS, Ahmed K. E-learning in surgical education: a systematic review. J Surg Educ. 2015;72(6):1145-1157.
-
Mortagy M, Abdelhameed A, Sexton P, et al; Egyptian Medical Education Collaborative Group (EGY MedEd). Online medical education in Egypt during the COVID-19 pandemic: a nationwide assessment of medical students’ usage and perceptions. BMC Med Educ. 2022;22(1):218.
- O’Leary FM. Paediatric resuscitation training: is e-learning the answer? A before and after pilot study. J Paediatr Child Health. 2012;48(6):529-533.
- O’Leary FM, Janson P. Can e-learning improve medical students’ knowledge and competence in paediatric cardiopulmonary resuscitation? A prospective before and after study. Emerg Med Australas. 2010;22(4):324-329.
- Veletsianos G, Houlden S. Radical flexibility and relationality as responses to education in times of crisis. Postdigit Sci Educ. 2020;2(3):849-862.
- DasGupta S, Fornari A, Geer K, et al. Medical education for social justice: Paulo Freire revisited. J Med Humanit. 2006;27(4):245-251.
- Migueliz Valcarlos M, Wolgemuth JR, Haraf S, Fisk N. Anti-oppressive pedagogies in online learning: a critical review. Distance Educ. 2020;41(3):345-360.
- Duke P, Grosseman S, Novack DH, Rosenzweig S. Preserving third year medical students’ empathy and enhancing self-reflection using small group “virtual hangout” technology. Med Teach. 2015;37(6):566-571.
- de la Harpe B, Radloff A. Lessons learned from three projects to design learning environments that support “generic” skill development. J Learn Des. 2006;1(2):21-34.
-
Jiménez-Cortés R, Aires L. Feminist trends in distance and hybrid higher education: a scoping review. Int J Educ Technol High Educ. 2021;18(1):60.
- Peacock S, Cowan J. Retreats for intramental thinking in collaborative online learning. Reflective Pract. 2017;18(1):1-13.
-
Lim BR. Guidelines for Designing Inquiry-Based Learning on the Web: Online Professional Development of Educators. Dissertation. Indiana University; 2001. Accessed October 2, 2023. https://www.proquest.com/openview/0c3bfbb9f2343b20e1b5df52d48431f1/1?pq-origsite=gscholar&cbl=18750&diss=y
- Magnussen L, Ishida D, Itano J. The impact of the use of inquiry-based learning as a teaching methodology on the development of critical thinking. J Nurs Educ. 2000;39(8):360-364.
-
Wood J, Levy P. There are more answers than questions: a literature review of questioning and inquiry-based learning. University of Lincoln; 2015. Accessed February 25, 2023. https://bpb-eu-w2.wpmucdn.com/blogs.lincoln.ac.uk/dist/f/1939/files/2015/07/JW-and-PL-Questioning-and-IBL-Literature-Review-final-July-20151.pdf
-
Vovides Y, Inman S, Rao D, Pongsajapan R, Burstein M. A model for reflective sensemaking: implementing Cohere in courses. Poster presented at: International Conference on Learning Analytics and Knowledge; April 8-13, 2013; Leuven, Belgium.
-
Lotrecchiano G, Vovides Y, Mallinson T, et al. Learning interventions for collaborative team science: preparing health and biomedical workers for success in collaborative teaming through reflective sensemaking. Paper presented at: GW Research Days; May 12, 2016; Washington, DC.
-
Christenbury L, Kelly PP. Questioning: a path to critical thinking. ERIC Clearinghouse on Reading and Communication Skills; National Council of Teachers of English; 1983. Accessed February 27, 2023. https://files.eric.ed.gov/fulltext/ED226372.pdf
-
Tofade T, Elsner J, Haines ST. Best practice strategies for effective use of questions as a teaching tool. Am J Pharm Educ. 2013;77(7):155.
- DeSapio J. Transformational learning: a literature review and call forward. J Transform Learn. 2017;4(2):56-63.
-
Eoyang GH. Human systems dynamics: complexity-based approach to a complex evaluation. In: Williams B, Imam I, eds. Systems Concepts in Evaluation: An Expert Anthology. EdgePress/American Evaluation Association; 2006:123-139.
-
Holladay R. Adaptive action: a tool for teaching and learning. Human Systems Dynamics Institute. September 2016. Accessed February 26, 2023. https://www.hsdinstitute.org/resources/adaptive-action-a-tool-for-teaching-and-learning-blog.html
- Guthrie KL, McCracken H. Teaching and learning social justice through online service-learning courses. Int Rev Res Open Distance Learn. 2010;11(3):78-94.
- Smith K, Jeffery D, Collins K. Slowing things down: taming time in the neoliberal university using social work distance education. Soc Work Educ. 2018;37(6):691-704.
- Fassetta G, Imperiale MG, Frimberger K, Attia M, Al-Masri N. Online teacher training in a context of forced immobility: the case of Gaza, Palestine. Eur Educ. 2017;49(2-3):133-150.
- Crutchfield J, Fisher AK, Plummer S. Best practices for antiracist education in virtual settings. Adv Soc Work. 2022;22(2):741-757.
- Herold DK. Mediating media studies—stimulating critical awareness in a virtual environment. Comput Educ. 2010;54(3):791-798.
- Breeze K, Holford N. Creating playful spaces for collaborative development of online teaching capacity. J Perspect Appl Acad Pract. 2021;9(2):91-100.
- Liu Y, Li D. Anti-oppressive research in group work. J Spec Group Work. 2023;48(2):128-145.
- Marcovitz DM. The intersection of social justice and educational technology: the educational technology social justice matrix. Educ Inf Technol. 2022;27(4):5129-5151.
- Maddamsetti J. Using body maps to understand elementary teacher candidates’ embodied understanding of care related to intersectional marginalization during the COVID-19 pandemic. Action Teach Educ. 2023;45(1):3-21.
-
Rothstein D. How can medical students learn to ask better questions? Right Question Institute. Accessed February 26, 2023. https://rightquestion.org/resources/medical-students-learn-questions-2/
-
Lai A, Lu L. Integrating feminist pedagogy with online teaching: facilitating critiques of patriarchal visual culture. Vis Cult Gend. 2009;4:58-68.
- Ukpokodu ON. Teachers’ reflections on pedagogies that enhance learning in an online course on teaching for equity and social justice. J Interact Online Learn. 2010;9(3):227-255.