Abstract
This article features images from the AMA Archives and brief narration of their importance for how Americans have oriented themselves to body habitus norms. In the early 20th century, the United States, as an industrialized nation with more food than ever, began to grapple with obesity. Questions about how to measure weight were being asked by the mid-20th century, as health professionals needed an indicator of obesity to accompany medicine’s attempts to help patients and populations control it as a health risk.
Measuring Weight
Body mass index, known colloquially as BMI, is currently the most familiar indicator of obesity, despite its known flaws.1,2 But how did it come to be, and how was obesity calculated and talked about before the BMI entered our lexicon? More specifically, how did America’s physicians think about it? This article examines the origins and flaws of BMI as an indicator of obesity and how physicians and medical organizations, including the American Medical Association (AMA), addressed weight management as part of health care before the 1970s, with specific attention to visual materials from the AMA archives.
A Brief History of BMI
Based on the work of mid-19th century scientist Adolphe Quetelet, BMI as we know it today (703 x weight (lbs)/[height (in)]2) was promoted by Ancel Keys in the July 1972 issue of the Journal of Chronic Diseases.3,4 Quetelet had initially designed the formula to study population averages and to identify the “type” or “ideal”4 (the ideal in this case being the average ratio of weight in kg to height in m2). Keys was moved to give the formula a second life after studying insurance companies’ height-weight tables and noting that they ignored body fat content, although it must be noted that the AMA was integral to the creation of these standards and participated in the first Adult Weight Conference in 1927.5 A compilation of articles and information on weight loss, edited by Morris Fishbein, then-editor of Journal of the American Medical Association, marks the first time the AMA addressed the issue for the public (see Figure 1). The timing was likely in response to the shift from food scarcity to food abundance, and for the first time being overweight was a problem for more than just the very wealthy.6
Figure 1. Table of Contents from Your Weight and How to Control It, by Morris Fishbein
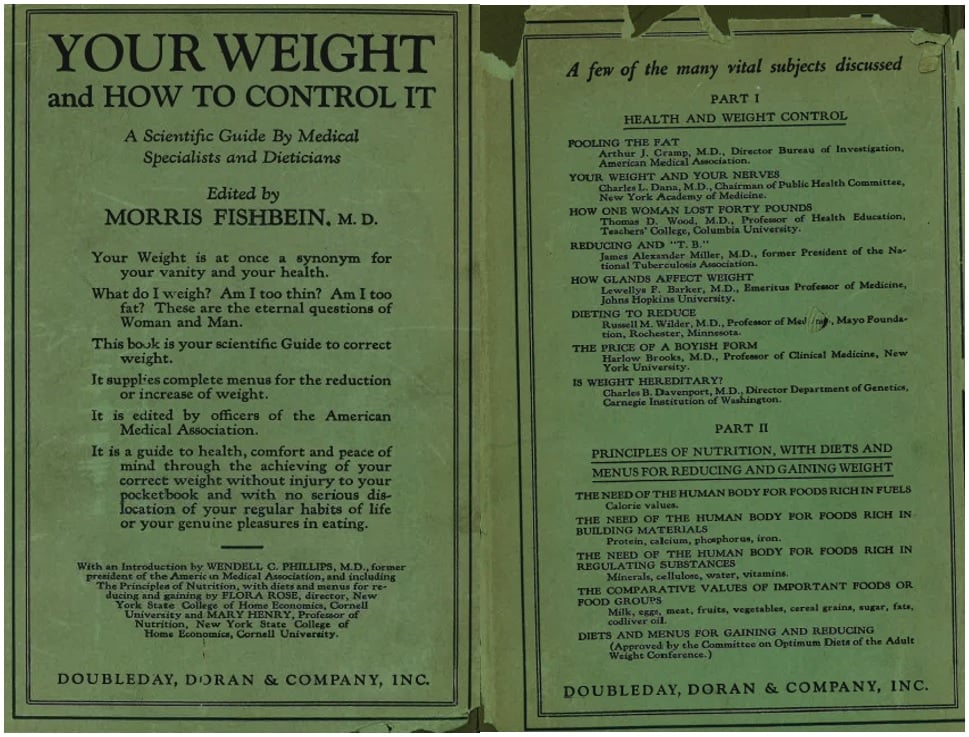
Reproduced fromFishbein.5
Ideal weight charts were created initially by life insurance firms, but, by 1926, the AMA and other health organizations were involved in their creation.5 The blue chart (Figure 2) is from a 1958 pamphlet titled “How to Lose Weight and Reduce Sensibly.” This title suggests that, at mid-century, the AMA’s main concern was unhealthy and fad dieting rather than obesity. It is also clear when comparing this chart to the ones printed in Fishbein’s book in 1927 (Figure 3) that obesity standards were already inching upwards, as was also shown in studies.7 While obesity itself was only recently labeled an epidemic7 and it was not until the 1990s that the extent of the obesity epidemic became clear,8 Keys himself warned of a coming obesity epidemic in the 1950s due to changes in the lifestyle and food options available to most Americans.1
Figure 2. Ideal Weights, 1958
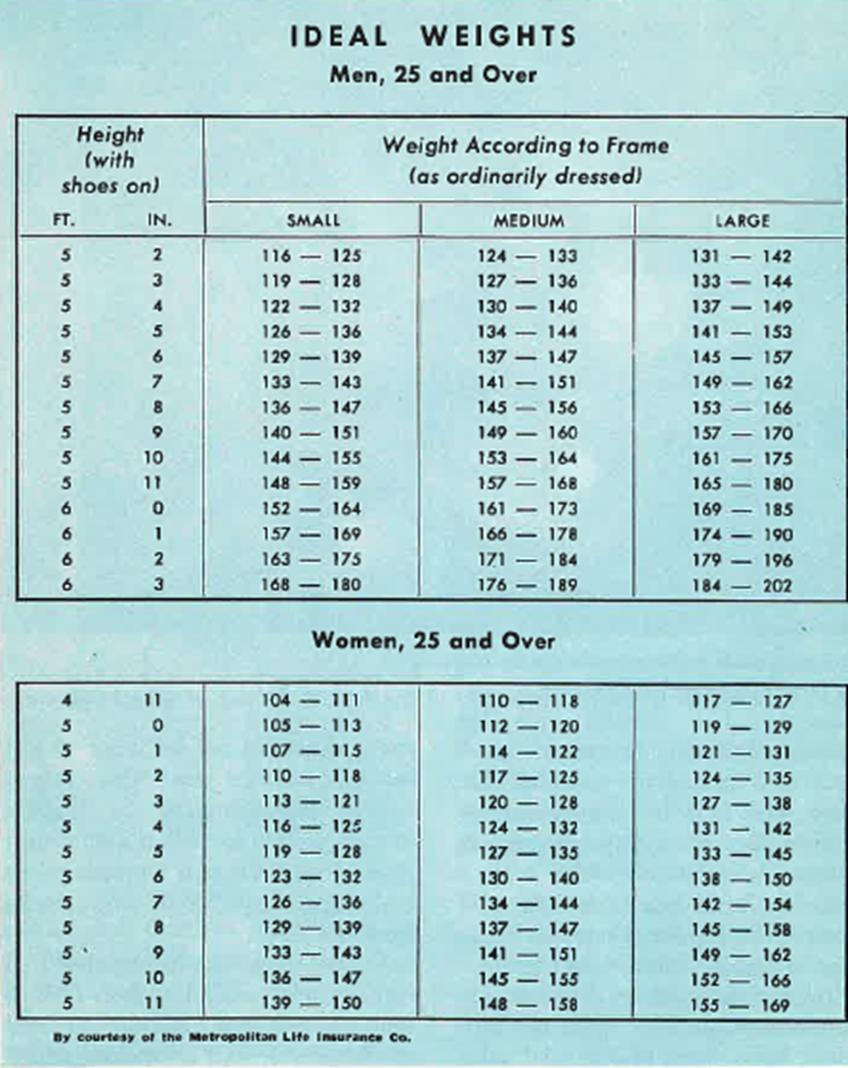
Courtesy of AMA Archives.
Figure 3. Male and Female Height-Weight Charts
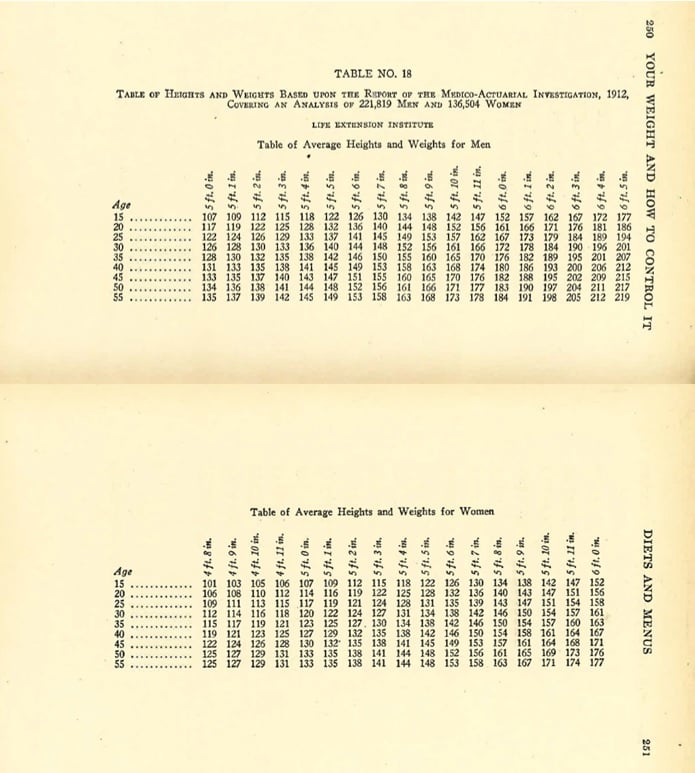
Reproduced from Fishbein.5
BMI as a measure of obesity is problematic. Not only does BMI have blind spots with regard to muscle mass and body fat, but it was based exclusively on Quetelet’s study of adult males and, in particular, Scottish and French soldiers.2 Although Keys did attempt to account for cultural and racial differences with his famous Seven Countries Study,9 BMI is notoriously unreliable as a rough measure of health for women and people of color.10 Finally, BMI categories are frequently stereotyped, as someone with a “normal” BMI is considered healthier than someone with a BMI that puts them in the obese category. This mode of thinking, however, disregards many things we now know about overall health, including that many people with obesity are metabolically healthy.11
The AMA Talks Weight
The AMA’s popular magazine, Hygeia, shows how, in the early days of the AMA’s discussion on achieving a healthy weight, the concern was primarily about young women starving themselves to achieve the ideal “flapper” figure (see Figure 4).
Figure 4. Illustration from “Dieting Daughters”
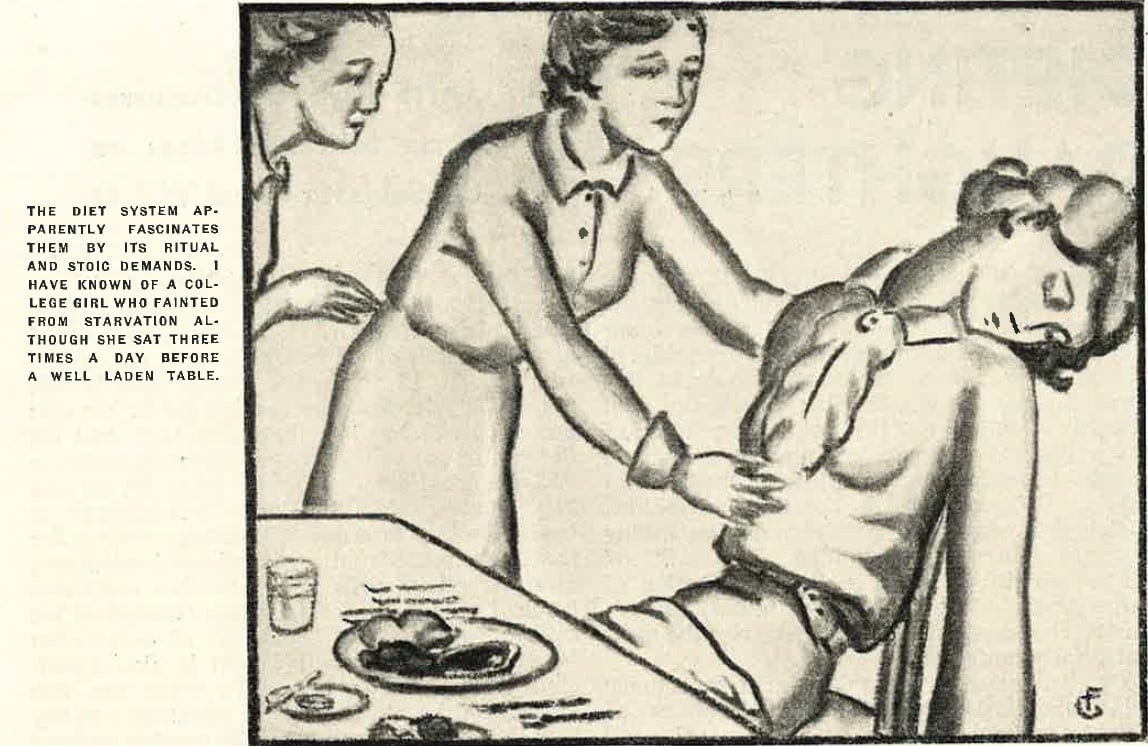
Reproduced from Foster.12
Despite repeatedly reminding readers that weight loss was a matter of good health and providing sensible, safe dieting advice, many of the AMA’s publications appealed to women’s perceived vanity and promoted the idea that a healthy weight was synonymous with beauty and status, thereby promoting one of the issues (unsafe dieting) it sought to prevent as well as advancing sexist stereotypes (see Figure 5).
Figure 5. Illustration from “And so You’re Reducing!”
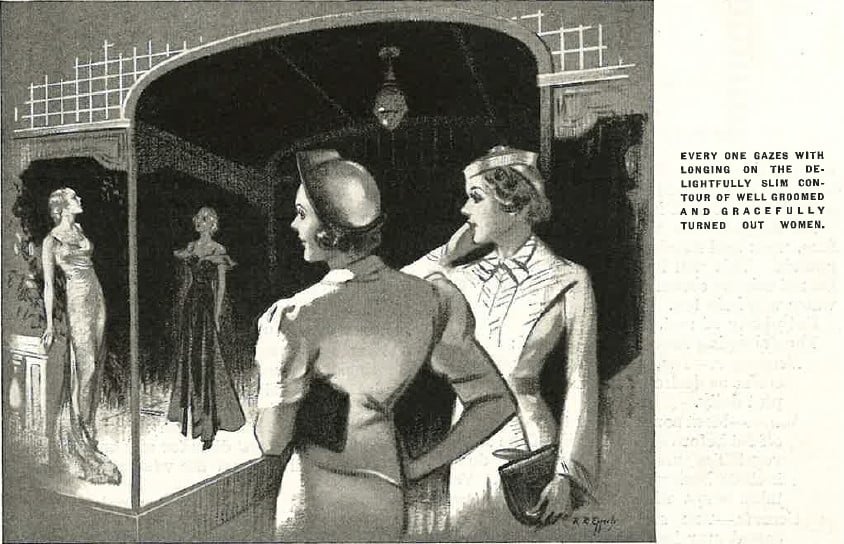
Reproduced from Geraghty.13
While we can see in Figure 4 that dieting to extremes was common in young women and something the AMA sought to put an end to, much of the AMA’s dietary advice at mid-century was aimed at mothers looking to help their daughters lose weight (see Figure 6). This messaging can set in motion a generational cycle of unhealthy attitudes toward food and internalized ideas about women as decorative objects.
Figure 6. Nutrition Is a Family Affair

Courtesy of AMA Archives.
Another public service poster from the 1950s highlights the ways that the AMA’s messaging around obesity and weight loss targeted women (see Figure 7).
Figure 7. Are You a Candidate for “Creeping Obesity”?
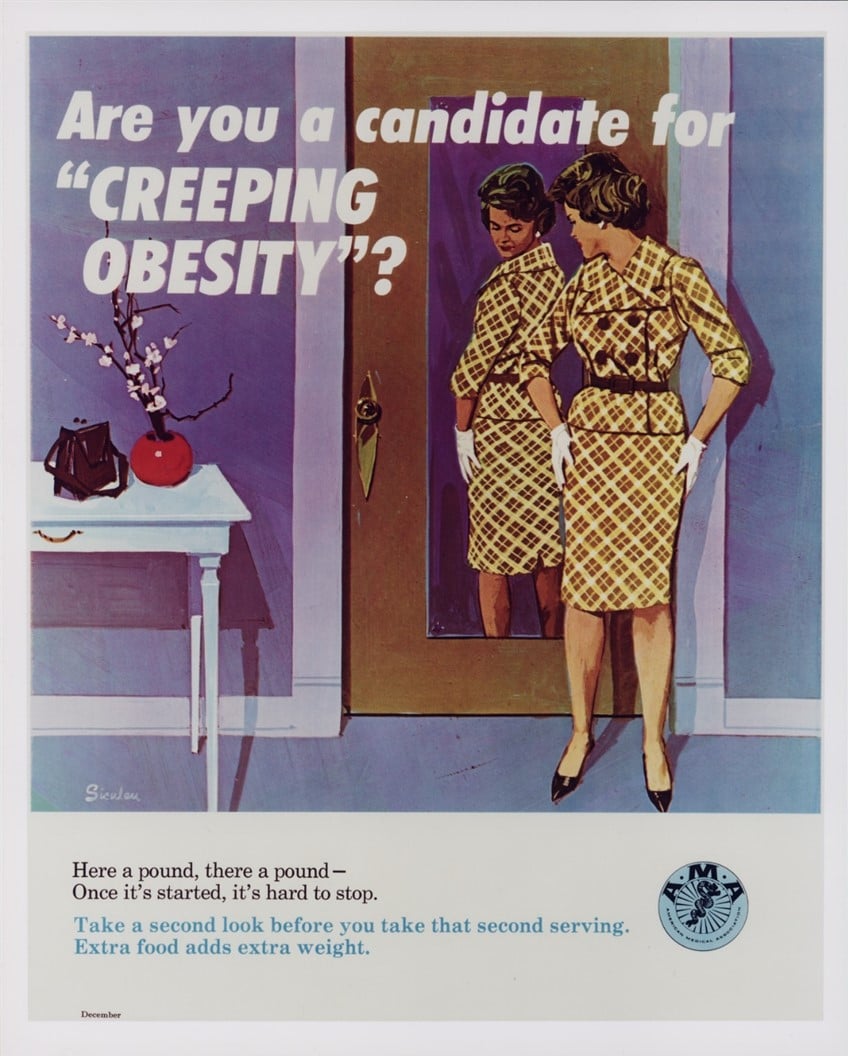
Courtesy of AMA Archives.
Given the unprecedented access to food (including processed food) created by the Second Industrial Revolution, it is perhaps unsurprising that dieting as we know it today began in the early 1900s.14 We can see this trend reflected in the literature of the 1920s, when the first public materials about weight gain and loss were created in response to both an increasingly heavy population and the surge in popularity of dangerous fad diets.15
At the time, calorie counting was seen as “rational,”14 and therefore those who were obese were irrational. This viewpoint is clear in the AMA’s framing of weight loss as a matter of simple self-control.14 The AMA also frequently used language of self-control that appealed to vanity rather than health outcomes, which may have contributed to the social stigma of obesity. Nowhere was this stigma more prevalent than in the ads targeting women, which made clear associations between thinness and desirability, as seen in Figure 5. Rare were images that focused on an overweight man (see Figure 8). Both the language and the image imply that overweight people are gluttonous and simply unwilling to take the hard steps needed to lose weight. Now we know that there are a number of biological, socioeconomic, and genealogical factors at play, but at the time (and still among some people), weight loss was viewed as a matter of willpower.
Figure 8. Illustration from “Can You Take It or Leave It?”
Reproduced from Walters.16
The AMA’s advice favored sensible diets with slow but steady weight loss over time and speaking to one’s doctor before embarking on a weight loss plan (see Figure 9). Looking back, the advice itself was sound, but the language and tone could be insensitive.
Figure 9. Me?!! Overweight?, 1955
Courtesy of AMA Archives.
Conclusion
It is only recently that an understanding of social determinants of health and the ways in which calorie restriction can slow our metabolism17 has altered the way that medical professionals talk to patients about weight loss. The problem of stigma still exists, though, and the way doctors speak to patients with overweight and obesity can lead to them foregoing medical care at all.18
The Metropolitan Life Tables’ criteria for defining obesity were widely used in the United States until the early 1990s when BMI came into vogue,19 so it is perhaps unsurprising that, despite known flaws in the way the medical profession talks about obesity, the practice continues.
In the 1970s, around the time that Keys was promoting Quetelet’s formula, obesity rates were going up, and American doctors were apparently getting fed up with patients’ supposed inability to stick to a sensible diet. At this time, factors like social determinants of health were unknown, and processed foods were only beginning to affect Americans’ health.8 In making weight loss seem simple and accessible (see Figures 10 and 11), the AMA inadvertently promoted the diet culture that exists in America to this day.
Figure 10. How to Kill Yourself
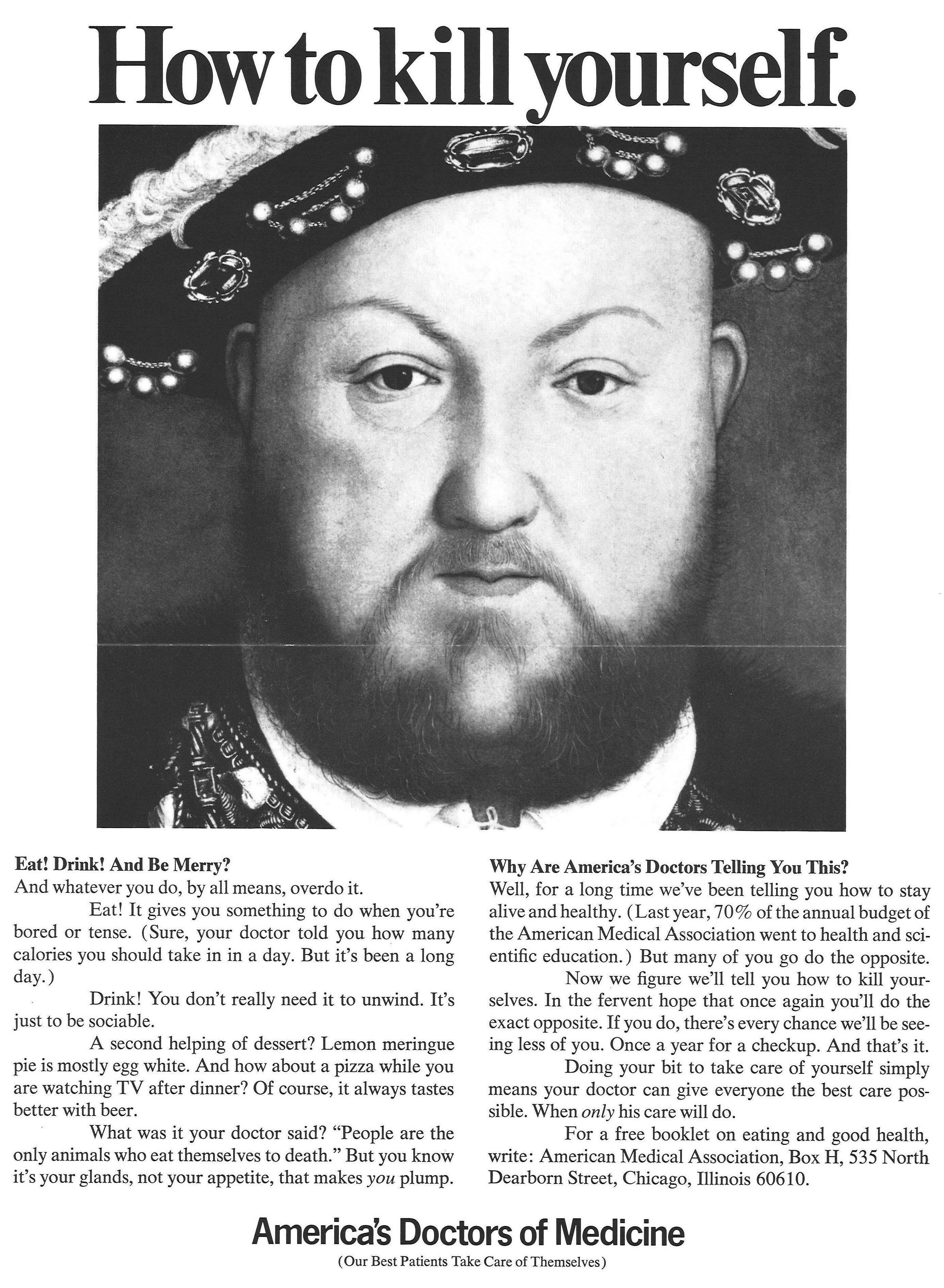
Courtesy of AMA Archives.
Figure 11. Don’t Walk When You Can Ride
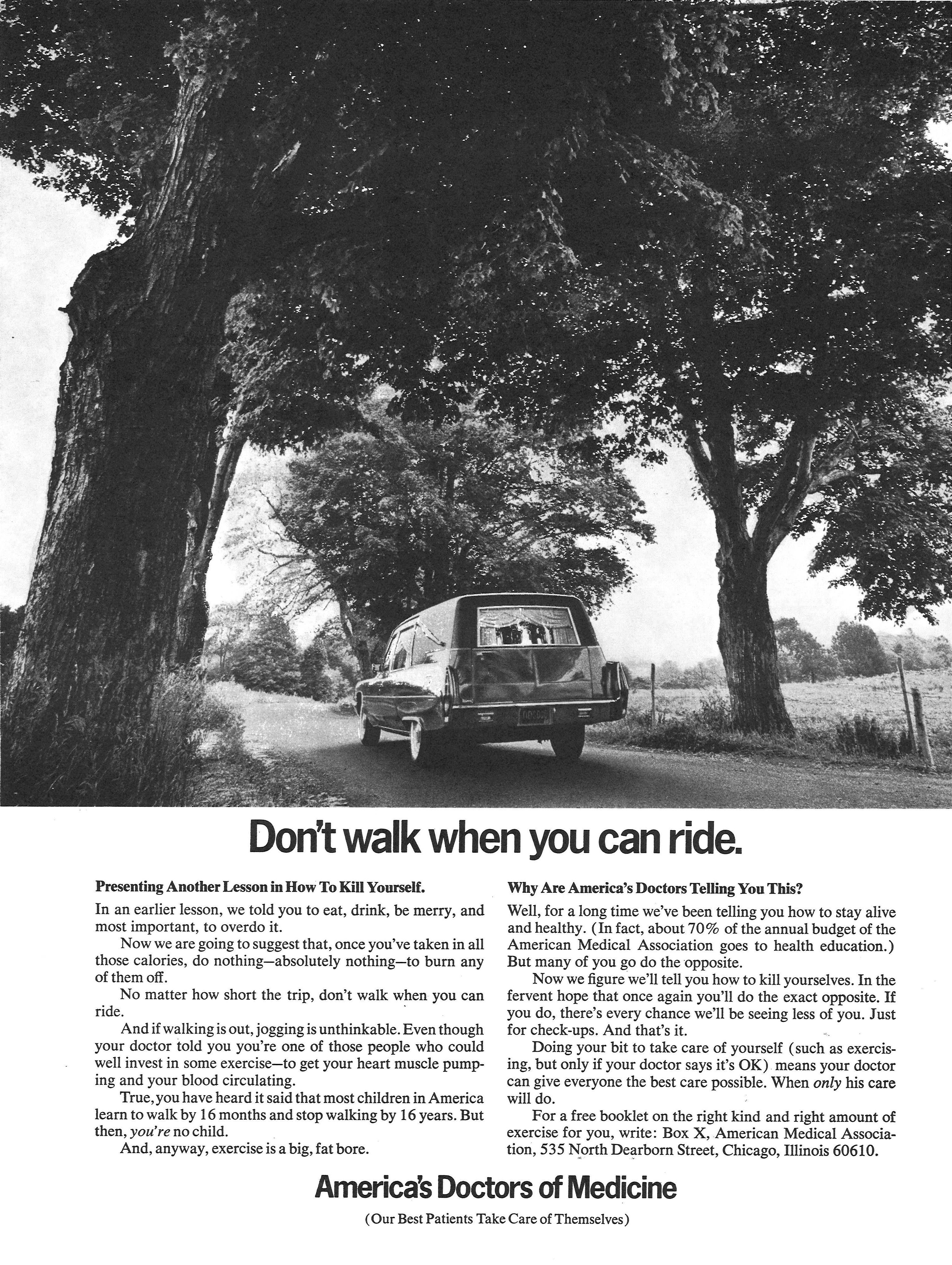
Courtesy of AMA Archives.
References
- Nuttall FQ. Body mass index. Nutr Today. 2015;50(3):117-128.
-
Tagle A, Schneider CM. Diet culture is everywhere. Here’s how to fight it. NPR. January 4, 2022. Accessed August 20, 2022. https://www.npr.org/2021/12/23/1067210075/what-if-the-best-diet-is-to-reject-diet-culture
- Blackburn H, Jacobs D. Commentary: origins and evolution of body mass index (BMI): continuing saga. Int J Epidemiol. 2014;43(3):665-669.
-
Stigler SM. The History of Statistics: Measurement of Uncertainty Before 1900. Harvard University Press; 1986.
-
Fishbein M. Your Weight and How to Control It. Doubleday Doran; 1927.
-
Segrave K. Obesity in America, 1850-1939: A History of Social Attitudes and Treatment. McFarland & Co; 2008.
- Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34(4):717-732.
-
Johnson SB. The nation’s childhood obesity epidemic: health disparities in the making. American Psychological Association. July 2012. Accessed August 20, 2022. https://www.apa.org/pi/families/resources/newsletter/2012/07/childhood-obesity
- Pett KD, Willett WC, Vartiainen E, Katz DL. The Seven Countries Study. Eur Heart J. 2017;38(42):3119-3121.
- Rahman M, Berenson AB. Accuracy of current body mass index obesity classification for white, black, and Hispanic reproductive-age women. Obstet Gynecol. 2010;115(5):982-988.
-
Phillips CM, Perry IJ. Does inflammation determine metabolic health status in obese and nonobese adults? J Clin Endocrinol Metab. 2013;98(10):E1610-E1619.
- Foster J. Dieting daughters. Hygeia. 1937;15(2):141-143.
-
Geraghty EM. And so you’re reducing! Hygeia. 1937;15(5):422-424.
- Jou C. The Progressive Era body project: calorie-counting and “disciplining the stomach” in 1920s America. J Gilded Age Prog Era. 2019;18(4):422-440.
-
Saner E. A history of diets—from Byron to 5:2. The Guardian. February 20, 2013. Accessed August 20, 2022. https://www.theguardian.com/lifeandstyle/2013/feb/20/a-history-of-diets-byron-52
- Walters PM. Can you take it or leave it. Hygeia. 1942;29(3):204-206.
-
Godoy M, Douglis S. Biology’s a b*tch: 5 reasons it’s so hard to keep weight off. NPR. May 1, 2019. Accessed August 7, 2022. https://www.npr.org/2019/04/25/717058877/the-biology-of-weight-loss
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319-326.
-
Komaroff M. For researchers on obesity: historical review of extra body weight definitions. J Obes. 2016;2016:2460285.