Abstract
Physicians tend to rely on diagnostic criteria, which can influence patients’ access to care by legitimizing need for care, connections to appropriate clinicians, and insurance coverage for indicated interventions. This article considers potential unintended but foreseeable negative consequences, including iatrogenic harm, of using body mass index (BMI) to distinguish typical from atypical anorexia nervosa, despite both illnesses sharing the same behaviors and complications. This article also suggests teaching strategies to help students learn to avoid overreliance on BMI in eating disorders care.
What Students Should Learn
Medical training and practice largely follow a “weight-normative approach,” which emphasizes weight management as an important aspect of health and well-being.1 This approach hinges on a widely held belief that higher body mass index (BMI) causes poor health. It is important for all health professions students to know that BMI, despite its omnipresence, is controversial. Abundant data suggesting complexity in relationships between BMI and health are often overlooked in clinical care. For example, one study found that when BMI categories were used to measure metabolic health, an estimated 75 million US adults were misclassified as cardio-metabolically healthy or unhealthy.2 A pedagogical upshot here is that diagnostic practices heavily reliant on BMI would benefit from additional specificity and precision. Especially when BMI cutoffs are used as diagnostic criteria, many clinicians and trainees may miss key health problems of a patient whose body habitus does not fit stereotyped illness presentation.
In this article, we consider potential unintended but foreseeable negative consequences, including iatrogenic harm, of using BMI to distinguish typical anorexia nervosa (AN) from atypical anorexia nervosa (AAN), despite both illnesses sharing the same behaviors and complications. We also suggest teaching strategies to help students learn to avoid overreliance on BMI in eating disorders care.
Bette’s Story
“I feel like if I had a smaller body right from the start, I would have gotten help when I was 15, when everybody started noticing I was losing a lot of weight and at 16, when I was vomiting blood” (E. Harrop, unpublished data, 2020).3 This quotation is from Bette (a pseudonym), a 38-year-old patient with AAN. Bette identifies as a nonbinary, white, pansexual, plus-sized US resident, who was low income as a child.3 Bette’s AAN developed in early adolescence; by age 15, they were eating less than 600 calories a day, purging multiple times daily, and losing weight rapidly, although never becoming “underweight” according to BMI (E. Harrop, unpublished data, 2020). After enduring multiple physical issues from their eating disorder (ED), including 2 pregnancies complicated by poor nutrition intake, a nurse practitioner finally questioned them about their ED, leading to a diagnosis at age 37. Their ED was severe and long-standing, warranting longer-term residential care, but insurance only approved 8 weeks of intensive outpatient care. At the time of this paper, Bette is still actively trying to recover from their decades-long battle with AAN, with suboptimal treatment supports.
Diagnosis and Treatment of EDs
In the case of AN, a hallmark symptom is emaciation with low BMI. Patients with AN in clinical vignettes are classically thin, with restrictive caloric intake, intense fear of weight gain and becoming fat, and disturbance in self-evaluation of body weight or shape. According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the severity of AN is classified mainly by BMI.4 However, not all patients engaged in severe self-starvation behaviors are emaciated.5 When patients, such as Bette, present with all of the symptoms of AN except emaciation (and have BMIs >18.5), they may be diagnosed with “other specified feeding and eating disorder” within the category of AAN. Despite their different classifications, AN and AAN have the same acute physiologic sequelae (bradycardia, low systolic blood pressure, low body temperature, and prolonged QTc interval on an electrocardiogram).6,7 There are few if any significant differences between patients with AN presentations who meet the low BMI criteria and patients who do not,7 leading some researchers to conclude that BMI is a poor predictor of AN severity7,8 and others to suggest that the BMI diagnostic criterion be removed from the DSM-5 to facilitate faster patient identification.3,9 Notably, one experimental study found that mental health trainees were significantly more likely to identify AN or AAN in a case study with an underweight patient than to identify AAN in identical patients with BMIs in the “normal” or “overweight” ranges,10 suggesting that patient BMI likely affects the diagnostic impressions and perceptions of clinicians. AAN can go undetected or undiagnosed because physicians are not primed to look for signs of starvation in patients with “normal,” “overweight,” or “obese” BMIs.
Although studies estimate the prevalence of AAN to be double or triple that of AN,11 in the United States, fewer patients with AAN than AN are referred to and admitted for ED-specific care.11 This disparity is consistent with the finding that patients with a BMI category of “overweight” or “obese” have 6 times lower odds of receiving inpatient medical care 1 year after diagnosis, despite experiencing greater percentages of weight loss.12 The second author (E.H.) found in a small study that, on average, patients with AAN experienced a treatment delay of 11.6 years.3 This treatment gap is crucial, because early identification and treatment of EDs is the best predictor of full recovery.13 Moreover, based on our clinical experience, categorization of an ED as AN or AAN affects approval for insurance coverage of intensive (often inpatient) treatment. Even when able to access care, patients have reported that their treatment experiences are often steeped in weight stigma and shaming comments from clinicians, who question their diagnosis, recommend weight loss, or prescribe restrictive diet plans.11,14 This overvaluation of BMI in ED treatment impedes referral, treatment, and recovery.11
Weight Stigma in Clinical Care
Medical training places significant emphasis on constructing differential diagnoses based on presenting symptoms. In practice, however, it is natural to fall back on heuristic methods and assess for diseases that match the clinical vignettes of one’s training (eg, screening for EDs in patients who are thin), but even manifestation of unconscious biases (eg, skipping screening for EDs in patients who are not thin) can reflect weight stigma—not only in one’s approach to care but also in one’s training.
Additionally, dominant representations in the media and in medical training tools narrowly frame patients with EDs as thin, young, and female, although patients with EDs are demographically diverse.15 One study based on surveys found that groups previously thought to be least at risk for EDs (eg, males, older individuals) demonstrated increases in the prevalence rates of some ED behaviors between 1998 and 2008.16 Moreover, people of lower socioeconomic status,17 people of color, and male-presenting individuals also present with EDs,18 and adolescents of lower socioeconomic status have been found to have higher rates of disordered eating behaviors than adolescents of high socioeconomic status.17 Representations of patients with EDs as young, female, cisgender, white, thin, and upper-middle class have the unintended consequence of making those who do not fit this dominant image—particularly due to intersecting marginalized identities—feel less welcome in treatment spaces. Reinforcement of damaging stereotypes can also make it harder for diverse patients to find services that meet their needs.19
Once identified as having AAN, patients often encounter weight stigma in clinical interactions. Like most of the general population, health care professionals harbor attitudes indicative of weight stigma,20 and medical trainees are no different.21 Clinician assumptions about eating behaviors based on BMI can harm rapport and make it harder for patients to be forthcoming about their disordered behaviors. In a study examining the health care experiences of patients with AAN, the second author (E.H.) identified multiple ways that patients felt weight stigma impacted their care and the course of their EDs.3 Among the physician behaviors patients viewed as harmful were the following: emphasizing weight or weight gain (particularly when patients were children), discounting or minimizing ED behaviors or symptoms, not believing patient reports of ED diagnoses or history, recommending weight loss or caloric restriction while the patient was in treatment for AAN, encouraging disordered eating behaviors (eg, skipping meals, compulsive exercise), and not referring patients to treatment after EDs were identified.3
Weight-Inclusive ED Care
The current recommendation is to treat atypical EDs as similarly as possible to the ED they most closely resemble (AN),22 but, in the case of AAN, the recommendation for sufficient daily caloric intake can contradict other medical guidelines, such as the recommendation that all patients with high BMIs be counseled to lose weight.23
As a field, mental health needs to get better at screening diverse individuals for EDs and providing weight-inclusive care that does not overly rely on BMI. Weight-inclusive approaches to care regard health and well-being as multifaceted; deemphasize weight; and focus on improving health behaviors (eg, nutrition quality and variety, sleep quality, enjoyable movement, meaningful social connections, participation in hobbies) and health care access and on minimizing weight stigma.1 While weight-inclusive approaches are important for ED-specific care, these approaches can also benefit other sectors of medicine, particularly sectors in which patients with EDs are likely to present (eg, primary care, emergency care, gastroenterology, internal medicine).
An ideal opportunity to emphasize these approaches is to incorporate more anti-weight stigma training in medical school curricula. Although variable amounts of education on EDs, nutrition, and obesity are included at each school,24 weight stigma is not uniformly addressed, even as implicit bias training is becoming a more prominent part of health professional education.25 Given the high rates of weight stigma reported in health care,26 a weight-inclusive approach is urgently needed in medical training. Additionally, medical training should include vignettes of patients with EDs that deviate from the accepted picture (for example, patients who are older, of higher weight, or persons of color). Strategies for weight-inclusive practices are also needed. Finally, while one-off seminars about weight stigma are useful, comprehensive curricular revisions can be necessary to create lasting changes in clinician attitudes.27
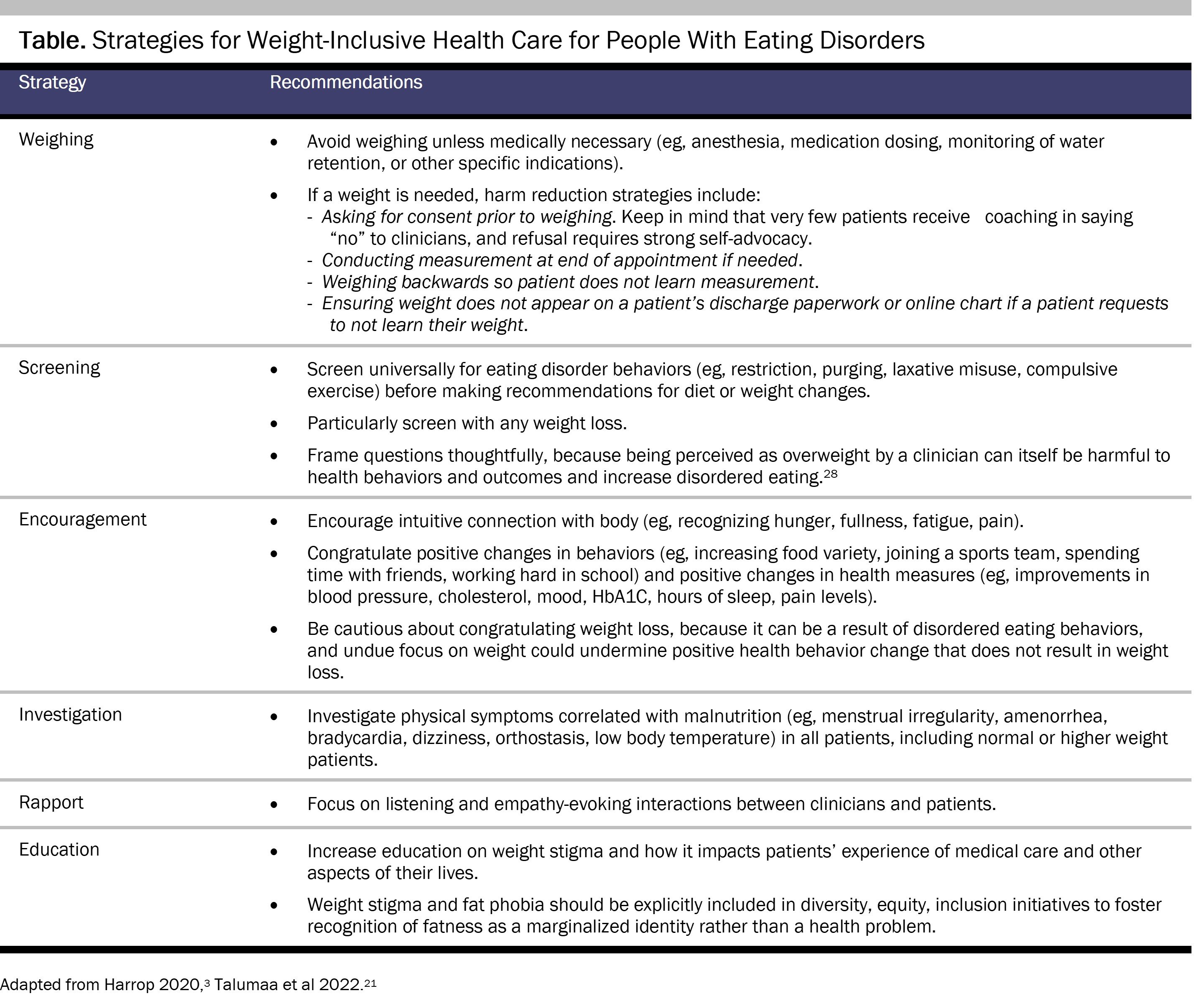
While research on weight-inclusive care, especially for EDs, is still in its infancy, researchers have made several recommendations for improving patient care across the weight spectrum (see Table).
Additionally, as current ED screeners lack predictive power29 and are not tailored to people across the weight spectrum, we propose a 2-question screener, based on our own clinical experience, to assess disordered eating and exercise behaviors in patients (regardless of BMI): (1) How do you feel about your body? and (2) Are you doing anything to try to change it (please specify)? We recommend these questions be asked with care, as questions about weight are sensitive and potentially stigmatizing (eg, “I recognize questions about eating habits and weight can be stressful, but it’s important for me to understand the pressures you might be facing”). Although testing of this screener is still in development, both authors have found (anecdotally) that this tool results in better identification of EDs in diverse patients; we recommend that screening for EDs occur after standard mental health screeners to allow for better rapport with patients.
Conclusion
Given the high prevalence of disordered eating behaviors, dieting behaviors, and concerns about body image,27,28 clinicians’ diligence and compassion in screening for EDs—even in patients they do not expect to struggle with these behaviors—will facilitate faster diagnosis and treatment. These efforts will validate the struggle with weight, diet, and appearance that many patients face and can even improve their quality of life and decrease the likelihood that they will have to wait years for appropriate care.
References
-
Tylka TL, Annunziato RA, Burgard D, et al. The weight-inclusive versus weight-normative approach to health: evaluating the evidence for prioritizing well-being over weight loss. J Obes. 2014;2014:983495.
- Tomiyama AJ, Hunger JM, Nguyen-Cuu J, Wells C. Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005-2012. Int J Obes (Lond). 2016;40(5):883-886.
-
Harrop EN.“Maybe I Really Am Too Fat to Have an Eating Disorder”: A Mixed Methods Study of Weight Stigma and Healthcare Experiences in a Diverse Sample of Patients With Atypical Anorexia. Dissertation. University of Washington; 2020. Accessed March 30, 2023. https://digital.lib.washington.edu/researchworks/bitstream/handle/1773/46576/Harrop_washington_0250E_22243.pdf?sequence=1&isAllowed=y
-
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013.
-
Gaudiani JL. Sick Enough: A Guide to the Medical Complications of Eating Disorders. Routledge; 2018.
- Whitelaw M, Gilbertson H, Lee KJ, Sawyer SM. Restrictive eating disorders among adolescent inpatients. Pediatrics. 2014;134(3):e758-e764.
-
Peebles R, Hardy KK, Wilson JL, Lock JD. Are diagnostic criteria for eating disorders markers of medical severity? Pediatrics. 2010;125(5):e1193-e1201.
-
Sawyer SM, Whitelaw M, Le Grange D, Yeo M, Hughes EK. Physical and psychological morbidity in adolescents with atypical anorexia nervosa. Pediatrics. 2016;137(4):e20154080.
- Harrop EN. A lived experience perspective on the classification of atypical anorexia nervosa. Int J Eat Disord. 2023;56(4):844-845.
-
Veillette LA, Serrano JM, Brochu PM. What’s weight got to do with it? Mental health trainees’ perceptions of a client with anorexia nervosa symptoms. Front Psychol. 2018;9:2574.
- Harrop EN, Mensinger JL, Moore M, Lindhorst T. Restrictive eating disorders in higher weight persons: a systematic review of atypical anorexia nervosa prevalence and consecutive admission literature. Int J Eat Disord. 2021;54(8):1328-1357.
- Kennedy GA, Forman SF, Woods ER, et al. History of overweight/obesity as predictor of care received at 1-year follow-up in adolescents with anorexia nervosa or atypical anorexia nervosa. J Adolesc Health. 2017;60(6):674-679.
- Lebow J, Sim LA, Kransdorf LN. Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. J Adolesc Health. 2015;56(1):19-24.
- Harrop EN. Typical-atypical interactions: one patient’s experience of weight bias in an inpatient eating disorder treatment setting. Women Ther. 2019;42(1-2):45-58.
- Mitchison D, Mond J, Bussey K, et al. DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychol Med. 2020;50(6):981-990.
-
Mitchison D, Hay P, Slewa-Younan S, Mond J. The changing demographic profile of eating disorder behaviors in the community. BMC Public Health. 2014;14:943.
-
Neumark-Sztainer D, Story M, Falkner NH, Beuhring T, Resnick MD. Sociodemographic and personal characteristics of adolescents engaged in weight loss and weight/muscle gain behaviors: who is doing what? Prev Med. 1999;28(1):40-50.
- Sonneville K, Lipson S. Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int J Eat Disord. 2018;51(6):518-526.
-
Harrop EN, LaMarre A. Painting pretty pictures of recovery: a critical discourse analysis of eating disorder treatment center promotional materials. J Adolesc Health. 2018;62(2)(suppl):S6.
-
Flint SW. Time to end weight stigma in healthcare. EClinicalMedicine. 2021;34:100810.
-
Talumaa B, Brown A, Batterham RL, Kalea AZ. Effective strategies in ending weight stigma in healthcare. Obes Rev. 2022;23(10):e13494.
- Wilson GT, Shafran R. Eating disorders guidelines from NICE. Lancet. 2005;365(9453):79-81.
-
Phelan S, Nallari M, Darroch FE, Wing RR. What do physicians recommend to their overweight and obese patients? J Am Board Fam Med. 2009;22(2):115-122.
-
Moore CH, Oliver TL, Randolph J, Dowdell EB. Interventions for reducing weight bias in healthcare providers: an interprofessional systematic review and meta-analysis. Clin Obes. 2022;12(6):e12545.
-
Cooper LA, Saha S, van Ryn M. Mandated implicit bias training for health professionals—a step toward equity in health care. JAMA Health Forum. 2022;3(8):e223250.
-
Himmelstein MS, Knepp KA, Phelan SM. The role of weight stigma in weight regain in bariatric surgery. Front Endocrinol (Lausanne). 2022;13:1076696.
-
Friedrich B, Evans-Lacko S, London J, Rhydderch D, Henderson C, Thornicroft G. Anti-stigma training for medical students: the Education Not Discrimination project. Br J Psychiatry Suppl. 2013;55:s89-s94.
- Haynes A, Kersbergen I, Sutin A, Daly M, Robinson E. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes Rev. 2018;19(3):347-363.
- Hay P, Hart LM, Wade TD. Beyond screening in primary practice settings: time to stop fiddling while Rome is burning. Int J Eat Disord. 2022;55(9):1194-1201.