Abstract
This article describes how size-based health and beauty ideals made their way into the medical field through the eugenics movement of the 19th to 20th centuries and were validated using so-called “standard weight” tables. They became even more mainstream with the 20th-century tool to replace standard weight tables: body mass index (BMI). BMI, then, is a continuation of white supremacist embodiment norms, racializing fat phobia under the guise of clinical authority. This article describes the key players in the legacy of size-based mandates, which fall under what I have labeled the “white bannerol of health and beauty.” This pseudoscientific bannerol has helped forge oppressive conceptions of fatness as an indicator of ill health and “low” racial quality.
Fat Fright
Today, we treat “obesity” (measured as a body mass index [BMI] ≥ 30) with a surprising seriousness, given its history. Fear of fatness did not begin as a medical concern. In fact, it took off in the mid-18th century. At that time, several race scientists began arguing that being “too fat” was bad specifically because it had been linked to women of color. Renowned scientist Georges-Louis Leclerc, Comte de Buffon, for instance, repeated claims made by other scientists that Chinese people while not all “fat and bulky … consider being so as an ornament to the human figure.” Adding that one could find, therefore, many Chinese women with enormously “big bellies.” Big bellies were also, according to Buffon, a noticeable deficit among the women of some African tribes.1
These ideas crept into medicine through eugenics. Eugenics was a late-19th to mid-20th century movement to promote so-called better breeding by identifying qualities of the human race to be cultivated and defects of the human population to be eradicated through selective breeding. Race and weight were intrinsic to their concerns. In the United States, eugenicists like the zoologist Charles Davenport argued that fatness was a constitutional flaw. The “low” types betrayed this form of embodiment. Chinese and Jewish people, for instance, were thought to be prone to a lamentable “racial obesity.”2
Davenport and other eugenicists, by combining race science and medical science, were inventing what I call a “white bannerol of health and beauty.” This bannerol pseudoscientifically bundles attractiveness and healthfulness. Peoples and physical proportions that had been held in high or low esteem by race theorists and philosophers of beauty were, with the eugenics movement, subject to a new form of medical penalty. These faux-scientific notions about body size, health, and desirability (especially for women) would ultimately make their way into the medical mainstream.
Insuring Against Fatness
Davenport had frontloaded race in his pseudoscientific understanding of the link between weight and health. He’d also embraced the latest science for identifying how much fat was believed to make a person sick. Such notions had arrived by way of the insurance companies.
The insurance industry had long been creating so-called “standard weight” tables. These tables gave the average weight by age and height for thousands of people judged by insurance companies’ medical examining boards to be sufficiently healthy to be acceptable life insurance risks.3 Most of the insured were white, but the insurance industry’s primary concern was not in identifying racial differences but in demonstrating a link between weight and health. This was the mechanism used to delimit potential policyholders and, by extension, potential monetary payouts. Yet the insurance industry’s ignoring race did not stop Davenport and others from continuing to make racialized assertions about body weight. Davenport was known to use the weight tables to advance his eugenic claims about a racial factor in obesity.4
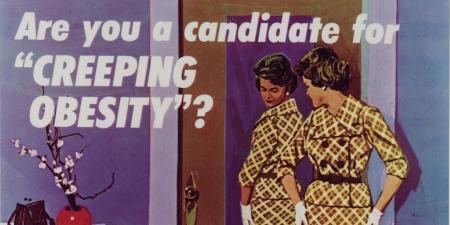
Still, as the 20th century wore on, eugenic claims were becoming less tenable. The devastation of the Holocaust led some postwar scientists to publicly admit that race was not biological.5 During the 1940s and 1950s, the medical community downplayed the overt role of race in questions of health, even those about obesity.6 A new emphasis was placed on discipling the bodies of all people based on the insurance industry weight tables, which unfortunately still relied on an implied white standard.
A 1951 paper titled “Obesity and Its Relation to Health and Disease” exemplifies this emphasis.7 Two of the 4 coauthors were affiliated with the insurance industry. The first author was Donald B. Armstrong, an esteemed physician recognized by the American Public Health Association (APHA) as one of the men who, in the early 20th century, “created the profession of public health.”8 A Charter Fellow of the APHA, Armstrong was also the vice president in charge of the Health and Welfare Program for the Metropolitan Life Insurance Company (MetLife). The second author, Louis I. Dublin, was vice president of and a statistician for MetLife. In their paper, the authors assert that “[o]ne of the subtler” and yet somehow “more serious health hazards of our time is obesity.”7 Presumably, it manages to be both subtle and serious because it lies “in the twilight zone between health and disease.”7 To estimate the number of US adults who were overweight or obese, they relied on “an arbitrary percentage departure from average weight for height” from MetLife’s ideal weight tables. These ideal weights were established by MetLife based on analyses of policyholders’ weight, morbidity, and mortality. As a “practical measure,” the authors define overweight as 10% above ideal weight and obesity, or “pathological overweight,” as 20% above the ideal weight. The policyholders were themselves overwhelmingly white, male, and middle class, meaning they were far from representative of all Americans.
There was only one study reviewed in their paper in which gender was mentioned. That study found that increases in body weight led to increases in blood pressure, with the biggest effects being seen among older people and women. Although the etiology of body size is complex, according to Armstrong et al, “simple unadulterated overeating is the basic cause in the majority of cases.” They make the additional, baseless allegation that “we are probably safe in saying that overeating accounts for the overweight in at least 95% of the cases.”7
Like Davenport, Keys’ concerns about fatness were shot through with white aesthetic priorities.
An eye-popping amount of what is being asserted in this paper has no scientific foundation whatever. The claims were made by people with medical degrees who worked for insurance companies that had the money and power to create medical dicta. Nevertheless, it did index something important in the evolution of weight-tracking as a form of health monitoring: a movement toward standardization that would only intensify the tacit whiteness of medical standards. By the 1970s, this form of white-washed medicine would reach its apex.
New Pseudoscience of Obesity
Ancel Keys was a Berkeley- and Cambridge-trained physiologist. He had worked on questions of how little nutriment humans needed to survive during the war years. By the 1950s, he’d turned to addressing the other end of the spectrum: how much food and fat were too much? In a 1953 review article, “Body Fat in Adult Man,” Keys and coauthor Josef Brožek found that though weight was regularly examined in its relationship to health, it was an unsatisfactory gauge of fatness: “[b]ody weight, even when evaluated with reference to the size of the skeleton, is a poor measurement of fatness.”9 Moreover, Keys and Brožek noted that “The practices followed in connection with the use of ‘standard weight’ tables vary in a most confusing way,” as people might be weighed with or without shoes and clothing. For example, to compensate for shoes and clothing, one author “subtracted 10 lb. from the weight and 1 in. from the recorded height of men,” and, for women, “the standard corrections were 6 lb. and 1.5 in.,” making the women appear on average heavier and shorter than men.9 Many of the early medico-actuarial tables used in studies of relationships between weight and health were “reproduced sometimes without citing the source or giving credit to Davenport.”9
Keys was ultimately prompted to look for a solution to the vagaries of the industry-born tables for measuring obesity. He landed on the Quetelet Index—renamed BMI, or kg/m2—and used it to determine the average build of men in a given country and how both the average and deviations from the average were linked to health conditions. He conducted a study that included working men from America and 5 European countries—Japan, which had been part of his notorious Seven Countries Study, was unceremoniously excluded. Keys found that BMI was not a better predictor of heart disease than other measures of relative weight or skinfold thickness—a commonly used measure of adiposity—for men from half the nations under study.10
Strangely, Keys declared the study a success. He claimed that BMI was preferable to other measures of obesity—like percent above average weight at a given height based on insurance industry tables—because it was “easy to calculate” and, unlike insurance tables, did not vary over time.10 That is, as noted by scholar Nicolas Rasmussen, Keys was eager to endorse “BMI without evidence of its predictive superiority” as it “did nothing at the time to clarify the contribution of obesity to heart disease—long his stated motive.”10
Keys, like Davenport before him, was interested in the question of fatness for reasons outside of health. Keys allegedly described obesity in the presence of his friends as “disgusting,” “a health hazard,” and “ethically repugnant.”10 He also claimed that “very fat” people were “clumsy and prone to accidents,”10 although the evidence to support this claim, too, is lacking. Like Davenport, Keys’ concerns about fatness were shot through with white aesthetic priorities. That is, they fell under the white bannerol of health and beauty. And while Keys did not issue specific directives for fat women, much of the literature had long focused on the greater obstacle that fatness posed for women’s (read: white women’s) health and beauty, following its centuries-old association with “grotesque” women of color—especially African and Chinese women.
Nevertheless, BMI was slow to take off. A series of international conferences to identify and understand overweight and obesity were initiated in 1973 by the National Institutes of Health.11 BMI finally came to prominence with the National Health and Nutrition Examination Survey (NHANES). In 1985, the NHANES II blended practices from the insurance industry (i.e, by relying on a percentile-based range of “acceptable” weights) with BMI, defining overweight as BMI of greater than or equal to the 85th percentile and obesity as BMI of greater than or equal to the 95th percentile, an approach that didn’t exactly honor Keys’ vision of uniformity.12 That same year, the US Department of Agriculture (USDA) combined forces with the US Department of Health, Education, and Welfare (HEW) to develop different BMI standards for “desirable weights” for men and women.12 Perhaps unsurprisingly, (and again, these studies almost exclusively concerned themselves with white people) the desirable BMI for women was lower than for men, with a BMI of approximately 25 to 26 for men and approximately 24 to 25 for women being deemed “overweight.”12 It wasn’t until 1995 that the World Health Organization, the USDA, and the HEW seemingly noticed that questions of “ideal” and “desirable” weights were laced with moral and aesthetic judgments and defined a BMI of between 18.5 and 24.99 as “healthy” for adults of all ages.6
It is not possible that these BMI standards were based on a representative sample of people across the earth and over time before they were applied globally. Although uniformity was always Keys’ goal, the pretension that these categories were applicable to all if (in some minor way) BMI predicts health risk of white persons was rooted in colorblind racism.
In any event, if the foregoing discussion reveals anything, it’s that the scientific method was at best loosely and rarely applied in the creation of weight-based health categories, and at worst skirted. Which is to say, obesity science has always been a (racist) form of pseudoscience that relies on statistical correlations based on a limited portion of humanity. Knowing this fact, whatever could be the rationale for keeping it alive?
References
-
Leclerc Buffon GL. Buffon’s Natural History: Containing a Theory of the Earth, a General History of Man, of the Brute Creation, and of Vegetables, Minerals, &c &c &c. From the French. With Notes by the Translator. Vol 4. HD Symonds; 1807.
-
Strings S. Fat as a floating signifier: race, weight, and femininity in the national imaginary. In: Boero N, Mason K, eds. The Oxford Handbook of the Sociology of Body and Embodiment. Oxford University Press; 2021:145-164.
-
Fishbein M, ed; Rose F, Henry M. Your Weight and How to Control It: A Scientific Guide by Medical Specialists and Dieticians. Doubleday, Doran, & Co; 1929.
- Mitchell HH. Overnutrition and obesity. J Clin Nutr. 1952;1(1):66-76.
-
Jacobson MF. Whiteness of a Different Color: European Immigrants and the Alchemy of Race. Harvard University Press; 1999.
-
Strings S. Fearing the Black Body: The Racial Origins of Fat Phobia. New York University Press; 2019.
- Armstrong DB, Dublin LI, Wheatley GM, Marks HH. Obesity and its relation to health and disease. JAMA. 1951;147(11):1007-1014.
- Wheatley GM. Donald Budd Armstrong. MD—1886-1968. Am J Public Health. 1968;58(11):2007-2009.
- Keys A, Brožek J. Body fat in adult man. Physiol Rev. 1953;33(3):245-325.
- Rasmussen N. Downsizing obesity: on Ancel Keys, the origins of BMI, and the neglect of excess weight as a health hazard in the United States from the 1950s to 1970s. J Hist Behav Sci. 2019;55(4):299-318.
-
History. World Obesity. Accessed February 2, 2023. https://www.worldobesity.org/about/about-us/history
-
Komaroff M. For researchers on obesity: historical review of extra body weight definitions. J Obes. 2016;2016:2460285.