Abstract
This commentary argues that financial incentives for employees who meet body mass index requirements reinforce healthism, a false and oppressive ideology. Healthism is the view that personal health is the vehicle of well-being and that health is achieved by taking personal responsibility for habit modification. Healthist views about body shape and body weight enforce oppressive norms and can lead to pernicious harms, especially to members of vulnerable groups. Overall, this article argues that persons and organizations ought not to label behaviors that influence body shape and weight in normative terms, such as “ideal” or “healthy.”
Case
X is a large employer looking to reduce number of employee sick days, optimize productivity, encourage adherence to its wellness program activities, and promote “ideal health behaviors.” Employees who engage in such behaviors, document them, and maintain a body mass index (BMI) at or below 25 will be eligible for reduced insurance premiums.
CR is an X employee with a BMI of 29 and learns after a “weigh in” at a wellness day event that this means she is “nearly obese.” CR has never considered herself unhealthy, maintains an overall diet that is about 90% plant-based, and participates in many recommended “ideal health behaviors.” CR sees the offer for reduced insurance premiums, views those savings as significant, but feels they are out of reach. CR feels demoralized about being asked by her employer to “weigh in,” about being described as “nearly obese,” and about her health being deemed not good enough for her employers’ insurance premium reductions.
Many employees have complained that 25 as the BMI cutoff is discriminatory, encourages body negativity, and expresses views of wellness that are fundamentally racist, sexist, and ableist and that might not be “healthy” at all for many of X’s employees. Others have submitted formal written complaints arguing that protected health information should never be used to financially incentivize any company’s vision of employee health and wellness.
Commentary
Should employers offer financial incentives for employees who monitor and report “ideal health behaviors”? Should employers offer financial incentives for employees who meet BMI requirements? In this commentary, I take issue with these practices as described in the case above, arguing that labeling behaviors that influence a person’s weight in normative terms contributes to a phenomenon called healthism, an ideology that emphasizes one’s personal responsibility for one’s own health. Engaging in practices that support healthism is morally wrong, because healthism ignores social factors that constrain individuals’ choices and reinforces oppressive social hierarchies. Thus, we ought not to label behaviors influencing a person’s weight in normative terms. This conclusion extends to companies offering financial incentives for employees who engage in “ideal” personal behaviors that may influence their weight. Additionally, as I will explain below, the use of BMI as a marker of health is fraught and ought to be avoided by company wellness programs.
Healthism is a term coined by sociologist Robert Crawford in his 1980 discussion of a then-emerging homeopathic “health consciousness” and its associated social movements.1 Crawford defines healthism as “the preoccupation with personal health as a primary—often the primary—focus for the definition and achievement of well-being; a goal which is to be attained primarily through the modification of lifestyles, with or without therapeutic help.”1 In other words, healthism is the view that personal health is the vehicle of well-being and that health is achieved through the modification of personal habits. Healthism locates the locus of moral and causal responsibility for health in the individual. For example, healthism would hold that quitting smoking is one’s personal responsibility (as is picking up the habit in the first place); one is morally culpable for their smoking habit because one’s health is one’s own responsibility.
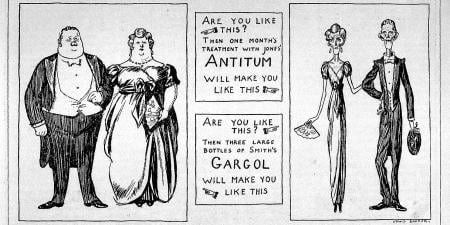
Healthism seems prima facie plausible. One’s health seems intricately connected to the choices one makes, and, in a very literal sense, one has control over one’s actions. With respect to smoking, one literally places the cigarette to one’s lips and lights the cigarette. With respect to something like diet and exercise, one literally controls the food that one puts in one’s mouth and the physical activities in which one engages. Healthism expresses what seems obvious: given that one’s actions influence one’s health, one would seem to be personally responsible for one’s health. Therefore, a company’s effort to incentivize certain behaviors that influence employees’ weight seems to make sense on its face—the company gives employees an incentive to engage in a certain “healthy” behavior, employees respond to the incentive by engaging in that behavior, and that behavior influences employees’ health. Some companies are very explicit about the connection between one’s health and one’s personal responsibility. For example, in 2010, Whole Foods launched an employee discount program wherein employees received greater discounts for meeting certain metrics, including BMI.2 Eleven years later, Whole Foods founder John Mackey publicly made healthist claims: “71% of Americans are overweight and 42.5% are obese. Clearly, we’re making bad choices in the way we eat.”3 Note the use of the normative term bad and the inference that Americans being overweight and obese is explained by the bad personal choices individual Americans make with respect to their diets. When companies promote certain behaviors as “ideal” and “healthy,” they reinforce similar healthist associations between certain behaviors and health: one can choose to smoke or not, and if one is unhealthy by virtue of smoking, it’s because one made a bad choice. Similarly, one can choose to eat certain foods, restrict others, and exercise a certain amount, so if one is obese, it’s because one has made bad choices.
Complicating Healthism
However, this healthist view is more complicated than it first appears. It’s true that in a very literal sense, individuals have control over the food they put in their mouths and the activities that their bodies do, much like it’s literally true that individuals control whether they light a cigarette or not. But the behaviors that we associate with smaller body shapes and lower body weights—cooking whole foods, eating lots of vegetables, going to the gym—are not equally accessible to all. These behaviors are influenced by social facts about a person. For example, one’s social class constrains the choices one can make. For example, author Barbara Ehrenreich describes trying to make ends meet while working in low-wage jobs like waitressing and hotel housekeeping.4 She discovered that if one can’t put up 2 months’ rent to secure an apartment, one must rely instead on a weekly rate motel and a hot plate, and one is forced to consume meals like fast food and gas station hot dogs regularly. Having fewer choices can lessen one’s agency and make one less morally culpable for one’s actions. Consider cases of coercion: we tend to see people who are forced to engage in some behavior and left with little or no choice as less morally culpable for that behavior. People whose health-related behaviors are constrained should be seen the same way.
Behaviors that we associate with smaller body shapes and lower body weights—cooking whole foods, eating lots of vegetables, going to the gym—are not equally accessible.
Even if a worker who earns low wages has an apartment, that worker might face challenges in engaging in the activities we associate with normative body shapes. Suppose a single mother has 2 jobs to make ends meet and provide for her children. When is she going to spend time preparing whole foods or shopping for whole foods? Is she going to be able to find childcare regularly so that she can go to the gym? If she is a single mother working 2 jobs, is she able to afford to shop for whole foods? Is she able to afford a gym membership? The social facts about this mom’s life constrain her choices in ways that can influence weight. So, it doesn’t seem as straightforward that the mom is morally culpable for “bad” choices because her options are limited.
Cases like the above are more common than one might think: a recent Brookings Institution report found that, across 373 metropolitan areas in America, between 30% and 62% of workers earn low wages.5 The challenges faced by workers earning low wages are compounded in vulnerable and marginalized groups. Workers earning low wages, although racially diverse, are disproportionately Latino/Hispanic or Black and disproportionately female.6 Forty percent of workers earning low wages aged 25 to 54 are raising children.6 Additionally, 12.8% of the US population lives in low-income and low-food-access areas, according to the US Department of Agriculture, and approximately half that group have limited access to a supermarket or grocery store.7 These food deserts are often inhabited by members of vulnerable groups: neighborhood racial segregation and poverty both independently reduce food store availability.8 Food deserts are more common in areas with lower levels of income and education and higher unemployment rates.9 The challenges of poverty, racial discrimination, child-rearing, and obesity often intersect, and these constraints are not accounted for by things like wellness programs that offer financial incentives for engaging in “ideal” health behaviors related to weight. Thus, wellness programs offering financial incentives for engaging in such health behaviors themselves entrench and compound social inequities.
Additionally, when doctors or wellness program directors say or imply that certain things like eating whole foods and exercising regularly will cause one to have an ideal body shape (and therefore improve one’s health), doctors and other institutional figures reinforce the idea that one can improve one’s metabolic health through behaviors for which one is personally, morally, and causally responsible. While this claim may be literally true with respect to one’s causal responsibility, it ignores possible social barriers to making behavioral choices, as discussed above. When an institution has a policy based on healthist views, that policy reinforces healthism’s power as an ideology by giving credence to healthism and penalizing employees who might have unseen constraints on the diet and exercise behaviors in which they can engage. Since healthism views people as morally responsible for their health behaviors, the implication that people who are fat fail to discipline themselves appropriately permits their being made targets of stigma and shame.10,11 If institutions ought not promote policies that reinforce oppressive social hierarchies, it follows that institutions shouldn’t promote wellness programs that incentivize engaging in “ideal” health behaviors related to weight.
Beyond BMI
The problems with using BMI as a metric to measure fatness are well documented; BMI fails to account for muscle mass12; BMI cutoffs for levels of obesity are arbitrary13; and, as a measure of overall health, BMI fails to account for differences in metabolic fitness between people with identical BMIs.14 Nevertheless, higher BMIs are associated with a higher risk for diseases like hypertension, coronary heart disease, respiratory illness, sleep apnea, and diabetes, among others.15 Higher BMIs are also associated with higher health care costs.16,17 If company wellness plans aim to reduce health care costs and the incidence of diseases comorbid with BMI, those plans could focus on behaviors like eating whole foods and exercising without referring to BMI itself. This seems like a reasonable proposal to me, as long as the modified wellness plans don’t use normative terms like ideal, good, or bad to label certain behaviors and instead refer to behavior in normatively neutral ways. For example, a plan could encourage fitness as a way to increase metabolic health and make clear, objective claims about the relationship between, say, fitness and heart disease or eating a plant-based diet and reducing one’s risk for cancer. These plans should also lower barriers to accessing things like fitness and whole foods in order to avoid reproducing social inequities. Lowering barriers might include more common forms of aid—group fitness classes, free gyms or gym memberships, providing whole foods in the workplace cafeteria—but they might necessarily involve other, uncommon forms of aid like free childcare so that employees have unencumbered time in which they can shop, prepare food, or exercise.
Company wellness programs that label some behaviors in normative terms like ideal or healthy can reinforce healthist ideology and reproduce social inequities. By avoiding labeling behaviors in normative terms, a company wellness plan can instead offer more objective information about the relationship between, say, diet and exercise and reducing one’s risk of disease. By employing nontraditional forms of aid, company wellness plans can also lower socially based barriers to the behaviors associated with reduced risk of disease and increased metabolic health.
References
- Crawford R. Healthism and the medicalization of everyday life. Int J Health Serv. 1980;10(3):365-388.
-
Brownstein J. Is Whole Foods’ get healthy plan fair? ABC News. January 27, 2010. Accessed February 13, 2023. https://abcnews.go.com/Health/w_DietAndFitnessNews/foods-incentives-make-employees-healthier/story?id=9680047
-
Clifford C. Whole Foods CEO John Mackey: the “best solution” is to not need health care and for Americans to change how they eat and live. CNBC. January 4, 2021. Accessed January 1, 2023. https://www.cnbc.com/2021/01/04/whole-foods-ceo-john-mackey-best-solution-is-not-to-need-health-care.html
-
Ehrenreich B. Nickel and Dimed: On (Not) Getting by in America. Metropolitan Books; Henry Holt & Co; 2001.
-
Ross M, Bateman N, Friedhoff A. A closer look at low-wage workers across the country. Brookings. March 2020. Accessed January 1, 2023. https://www.brookings.edu/interactives/low-wage-workforce/
-
Ross M, Bateman N. Meet the low-wage workforce. Brookings; 2019. Accessed January 1, 2023. https://www.brookings.edu/wp-content/uploads/2019/11/201911_Brookings-Metro_low-wage-workforce_Ross-Bateman.pdf
-
Rhone A, Ver Ploeg M, Dicken C, Williams R, Breneman V; Economic Research Service. Low-income and low-supermarket-access census tracts, 2010-2015. Economic Information Bulletin 165. US Department of Agriculture; 2017. Accessed February 3, 2023. https://www.ers.usda.gov/webdocs/publications/82101/eib-165.pdf?v=3395.3
-
Bower KM, Thorpe RJ, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med. 2014;58:33-39.
-
Exploring America’s food deserts. Annie E. Casey Foundation blog. February 13, 2021. Accessed January 1, 2023. https://www.aecf.org/blog/exploring-americas-food-deserts
-
Guthman J. Weighing In: Obesity, Food Justice, and the Limits of Capitalism. University of California Press; 2011.
- Eller GM. On fat oppression. Kennedy Inst Ethics J. 2014;24(3):219-245.
- Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond). 2008;32(suppl 3):S56-S59.
- James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9(suppl 4):228S-233S.
-
Ward M. Are coronavirus triage protocols sacrificing fat people? Should they? Int J Fem Approaches Bioeth Blog. May 5, 2020. Accessed January 1, 2023. http://www.ijfab.org/blog/2020/05/are-coronavirus-triage-protocols-sacrificing-fat-people-should-they/
-
Jensen MD, Ryan DH, Apovian CM, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Circulation. 2014;129(25)(suppl 2):S102-S138.
- Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff (Millwood). 2002;21(2):245-253.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood). 2009;28(5):w822-w831.